Rethinking Translational Research to Bridge the Gap between Science and Clinical Application
1Amhara Public Health Institute, Bahir Dar, Ethiopia
*Corresponding Author: Gizachew Yismaw: Email: gygiz62@gmail.com, Bahir Dar, Ethiopia,
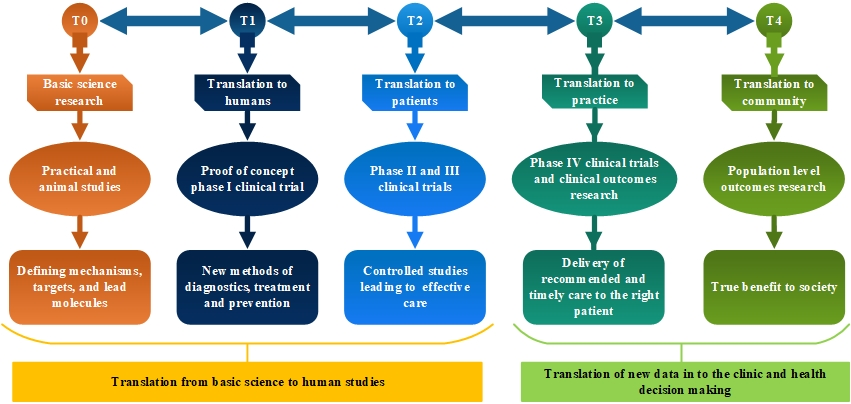
Translational research, and translational science have been used to describe the systematic effort to convert basic research outputs into practical applications to enhance human health and well-being. Generally, the use of translational research is harnessing knowledge from basic medical science and bringing it into clinical practice (so-called bench-to-bedside models). In the past, basic, clinical, and community-based researchers operated in separate domains, often creating barriers to the translation of scientific findings into widespread improvements in human health and implementing changes in the health care system. Translational research is aimed at translating (converting) results in basic research into results that directly benefit humans (1,2)
The evolution of medicine and medical technology hinges on the successful translation of basic science research from the bench to clinical implementation at the bedside. Substantial leaps in improving global health, such as antibiotics, vaccinations, and cancer therapies, have all seen successes under this paradigm, yet today, it has become increasingly difficult to realize this ideal scenario. Researchers have been forced to abandon time and resource consuming translational research to focus on publication generating work to maintain funding and professional advancement. Compared to the surge in scientific innovation and new fields of science, realization of transformational scientific findings in device development and materials sciences has significantly lagged.
Evidence-based practice can be conceptualized as clinical decision making that considers the best available evidence, the context in which the care is delivered, client preference and the professional judgment of the health professional.
The major components of the evidence-based healthcare process are healthcare evidence generation, evidence synthesis, evidence transfer and evidence utilization. Evidence-based healthcare is a cyclical process that derives questions, concerns, or interests from the identification of healthcare needs by clinicians or patients/consumers and then proceeds to address these questions by generating knowledge and evidence to meet these needs effectively and appropriately in ways that are effective, feasible, and meaningful to specific populations, cultures, and settings. This evidence is then appraised, synthesized, and transferred to service delivery settings and health professionals who then utilize it and evaluate its impact on health outcomes, health systems, and professional practice.
The challenges related to facilitating the cycle of scientific discovery through to the widespread adoption of a healthcare innovation have become of central concern to individuals and communities who seek or need healthcare; health professionals; policy makers and the funders of health services. Multiple, interacting reasons can be given for the general failure of health research findings to translate into practice (3), including historical, political, social, economic, scientific, cultural, and organization factors that slow or impede transfer of research into practice(4,5).
Today’s clinician-scientist needs the tools to both conduct translational research and implement those findings to continuously improve patient health, through the health care system and in the larger population. As we rethink the dogma of scientific research around the world, we must embrace the new paradigm of translational research and realize that the journey begins and ends at the bedside. As a health-care community, we must approach our practice honestly to admit and identify shortcomings of our care so that we may turn to our applied-scientist or clinician-scientist colleagues for solutions to these shortcomings. As a scientific community, we must open our system to integrated inter-institutional, multidisciplinary collaborations where we acknowledge and reward those undertaking the brave task of developing solutions, rather than more questions. As administrators, and mentors, we must continue to invest in the new wave of researchers who may not fit into the traditional paradigm of academic advancement and support the long road of work they have before them. As government agency, we must continue to build partnerships with the private sector to harness the strengths of all parties.
Translational research:
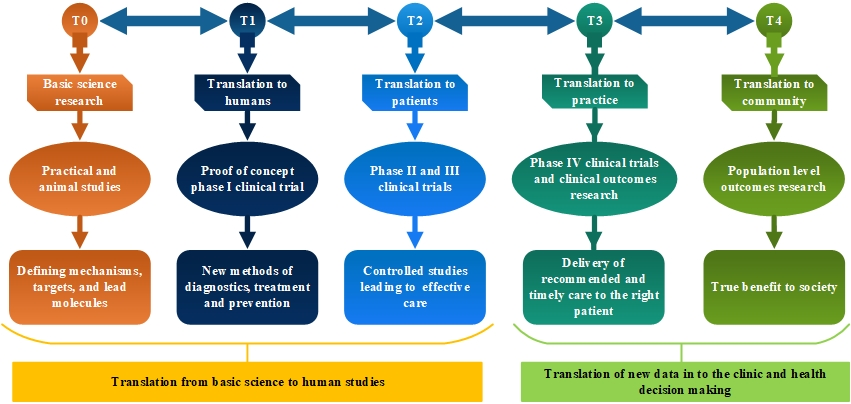
In summary, Translation is the process of turning observations in the laboratory, clinic and community into interventions that improve the health of individuals and the public from diagnostics and therapeutics to medical procedures and behavioral changes. Whereas translational science/ translational research is the field of investigation focused on understanding the scientific and operational principles underlying each step of the translational process
Herein, we recommend knowing how the current scientific paradigm struggles in the new healthcare landscape, the obstacles met by translational researchers, and solutions, both public and private, to overcoming those obstacles. We must rethink the old dogma of academia and reinvent the traditional pathways of research to truly impact the health care arena and ultimately those that matter most, the patient. Lastly, as a medical community, we must embrace each other with a solitary unifying goal to act on behalf of our patients and provide solutions to their unsolved clinical needs.