Figure 1 Map of the Amhara region by zone; war conflict-affected zones
Impacts of the Northern Ethiopian Conflict on Malaria Elimination Programs in the Amhara region, Northwest Ethiopia: A Time-Series Analysis
1Amhara Public Health Institute, Bahir Dar, Ethiopia
2School of Public Health, College of Medicine and Health Sciences, Bahir Dar University, Bahir Dar, Ethiopia
3Department of Pharmacy, College of Medicine and Health Sciences, Bahir Dar University, Bahir Dar, Ethiopia.
*Corresponding Author: Mastewal Worku, Tel: +251 943609027, e-mail matewal.worku@gmail.com,
Background: Malaria remains a significant public health challenge in the Amhara Region of Ethiopia. The armed Northern conflict from 2020 to 2022 significantly impacted the Amhara region, including driving internal displacement and disrupting healthcare services. This report aimed to assess the pattern of malaria epidemiology and the impact of war on elimination programs in conflict-affected zones of the Amhara Region.
Methods: Retrospective data, cross-sectional interrupted time-series analysis, and a project model were used to estimate the impact and calculate the relative level changes from 2020 to 2022. The model was validated by comparing the results with observed malaria incidence data.
Results: Although most health institutions have restored malaria services, they are still 24% below the pre-war levels, with up to 35 weeks of treatment interruptions occurring in conflict-affected areas and significant decreases in other zones. Malaria cases reported in 2021 surpassed those from 2018–2020, reaching 2020 levels, which is concerning because of continuous service interruptions. The number of confirmed cases increased across all district categories, with non-affected districts experiencing a proportionally larger increase than conflict-affected districts. Significant damage to malaria elimination supplies occurred in conflict-affected areas, especially North Shewa and South Wollo, leading to increases in cases. Ordinary least squares regression analysis further indicates a general decline in relative incidence ratios across conflict-affected districts, underscoring the impact of conflict on malaria control efforts.
Conclusions: A significant decline from pre-war levels and ongoing service disruptions in conflict-affected areas fuel malaria transmission, reactivation, and failed elimination. These calls for malaria elimination programs and vigilance surveillance systems for community screening, active case detection and effective management, and epidemiological studies to monitor the transmission dynamics.
Keywords: malaria, incidence, ITS, elimination, war, impact, Amhara Region
የጥናቱ ዳራ፡ ወባ በአማራ ክልል በማህበረሰብ ጤና ላይ ከፍተኛ ጉዳት የሚያስከትል ዋና የተላላፊ በሽታ ነው። ግጭት የወባ ስርጭትን የሚያባብሱ ነገሮች መካከል አንዱ ሲሆን፣ በክልሉ እ.ኤ.አ. ከ2020 እስከ 2022 የተካሄደው የሰሜን ኢትዮጵያ ግጭት የወባ መከሰትን እና የሞት መጠንን በከፍተኛ ሁኔታ አሳድጓል። የሆኑት ምክንያቶች በጤና ተቋማትና ባለሙያዎች ላይ የሚደርስ ቀጥተኛ ጥቃት፣ የመድኃኒት አቅርቦት እና ተደራሽነት ውስንነት፣ እንዲሁም የሚሊዮኖች የሰዎች መፈናቀል እና የታማሚዎች የህክምና ተደራሽነት መቋረጥ ይገኙበታል።
የጥናቱ ዓላማ ፡- ይህ ጥናት በክልሉ የወባ ስርጭት ሁኔታን እና ግጭቱ በወባ መከላከል እና መቆጣጠር ፕሮግራም ላይ ያሳደረውን ተፅእኖ በሳይንሳዊ መሰረት ያለ ምርጫዎችን በመግለጽ ያተኮረ ነው።
ዘዴዎች፡- የጥናቱ አሰራር በክልሉ የህብረተሰብ ጤና አደጋዎችና ስጋቶች አስተዳደር (PHEM) ዳታቤዝ ውስጥ ከሚገኙ የተቀመጡ የኋላ ታሪክ መረጃዎች ላይ ተመስርቷል። የጥናቱ ዓላማው ከጊዜ ከግጭቱ በፊትና ከግጭቱ በኋላ የነበረውን የክልሉ የወባ መከላከል እና መቆጣጠር የአፈፃፀም ሁኔታ ለመረዳት እና ግጭቱ በፕሮግራሙ ላይ ያሳደረውን ተፅእኖ ለመገምገም ነበር። አመታዊ የወባ ክስተቶች ትንበያ፣ የፕላዝሞዲየም ፋልሲፓረም መጠን (ፒኤፍ)፣ እንዲሁም በክልሉ አጠቃላይ የወባ ህሙማን ስርጭትን የሚያሳዩ ከሃያ ዓመት በላይ የተሰበሰቡ የወባ መረጃዎች ጥቅም ላይ ውለዋል። የተገኘውን ሞዴል ትክክለኛነት ለመሞከር የሞዴሊንግ ውጤቶቹ ከትክክለኛ የወባ ክስተት መረጃ ጋር ተነጻጽሯል። የወባ ህሙማንን ስርጭት አዝማሚያ ለመተንተን "ተንቀሳቃሽ አማካኝ" የሚባል ቀላል የማለስለስ ዘዴ ተተግብሯል። ውጤቶቹ በካርታዎች፣ ግራፎች እና የመስመር ግራፎች ጥቅም ላይ ውለዋል።
የጥናቱ ውጤት፡ ከግጭቱ በኋላ፣ ከሚጠበቅባቸው የወባ አገልግሎት አቅራቢ የጤና ተቋማት 77% (ከ 3,571 ጤና ኬሎች ውስጥ 2,751)፣ 79% (ከ 866 ጤና ጣብያዎች ውስጥ 684) እና 78% (ከ 81 ሆስፒታሎች ውስጥ 63) ብቻ የወባ አገልግሎት እንደሰጡ ተረጋግጧል። አጠቃላይ የወባ አገልግሎት አቅርቦት ከግጭቱ በፊት ከነበረው ደረጃ በ24% ቀንሷል። በተለይም በግጭት የተጎዱ አካባቢዎች ውስጥ እስከ 35 ሳምንታት ያህል የህክምና አገልግሎት ተቋርጦ እንደነበር ተረጋግጧል። በክልሉ በ2021 ዓ.ም የተመዘገበው የወባ ክስተት ከ2018 እስከ 2020 ዓ.ም ከነበረው በእጅጉ ከፍ ብሎ ከፍተኛ ከፍተኛ ደረጃ ላይ ደርሷል። በግጭቱ ያልተጎዱ ወረዳዎች በግጭት ከተጎዱ ወረዳዎች በተመጣጣኝ ጭማሪ አሳይተዋል። ግጭት በተከሰተባቸው አካባቢዎች በተለይም በሰሜን ሸዋ እና በደቡብ ወሎ በወባ መከላከያ አቅርቦቶች ላይ ከፍተኛ ጉዳት በማድረስ የችግሮች መጨመር አስከትሏል። የግጭት ሁኔታ በወባ ቁጥጥር ላይ ያለውን ተጽእኖ በማሳየት በግጭት በተጎዱ ወረዳዎች መካከል ያለው አጠቃላይ አንጻራዊ የመከሰቱ መጠን ማሽቆልቆሉን ያሳያል።የተጎዱ ወረዳዎች ከግጭት ጋር ሲነፃፀሩ በተመጣጣኝ ከፍተኛ ጭማሪ አላቸው።
የጥናቱ ማጠቃለያ፡ በግጭቱ በተጎዱ አካባቢዎች የወባ መከሰት በከፍተኛ ደረጃ ነበር። በግጭቱ የተጎዱ አካባቢዎች ውስጥ የጤና አገልግሎት መቋረጥ እየቀጠለ የመጣ ቢሆንም፣ ባልተጐዱም በሁለቱም አካባቢዎች የወባ ህሙማን ቁጥር ተስፋፍቶ ነበር። ይህ መቋረጥ የወባ ክስተት በግጭት በተጎዱም ሆነ ባልተጎዱ ወረዳዎች ውስጥ በእኩል እንዲስፋፋ አስተዋጽኦ አድርጓል። ሰለዚህ የተጠናከረ የልየታ እና የቅኝት ዘመቻዎች፣ የጤና መሠረተ ልማት መልሶ ግንባታ፣ እንዲሁም የወባ መከላከል እና መቆጣጠር ዘዴዎችን ማጠናከር ለክልሉ የወባ በሽታ ቁጥጥር መርሃግብር ለማሻሻል አስፈላጊ የሆኑ ስትራተጂዎች ናቸው።
ቁልፍ ቃላት፡- ወባ፣ ክስተት፣ መከላከል እና መቆጣጠር፣ ግጭት፣ ተፅእኖ፣ የአማራ ክልል
Malaria is a serious, life-threatening disease transmitted by the bite of an infected female Anopheles mosquito, which introduces the Plasmodium parasite into the human bloodstream (1). The five species of Plasmodium that are known to cause malaria in humans are Plasmodium falciparum, Plasmodium vivax, Plasmodium malariae, Plasmodium ovale, and Plasmodium knowlesi (2, 3).
Since the 1969 global malaria eradication campaign, several countries have implemented programs aimed at eliminating malaria (4). Elimination involves reducing locally acquired infections to zero, with ongoing measures to prevent re-establishment (5). Detections trigger a thorough investigation, classification, and response, ensuring effective transmission prevention (6). Malaria remains one of Ethiopia's major public health concerns despite the country's national malaria elimination program (NMEP), which has achieved significant progress in the fight to eliminate the disease and is committed to eliminating it by 2030 (7, 8).
Ethiopia’s malaria epidemiologic patterns are unique in comparison to other sub-Saharan African settings due to the high variability in the country’s geography and the co-endemicity of both Plasmodium falciparum and P. vivax (9). A total of 1,509,182 malaria cases were reported in 2020, with a general downward trend in the six years (10). The most recent malaria indicator survey, conducted in 2015, estimated an overall parasite prevalence among all ages of 0.5%, with regional rates reaching up to 12 times higher, particularly in the western lowlands (11).
War significantly impacts malaria risk by driving migration, collapsing health services, restricting access to treatment, fostering drug and insecticide resistance, reducing immunity, and increasing exposure to mosquitoes due to poor housing and environmental degradation (12). Many conflicts occur in countries with high malaria incidence; for instance, the Afghan civil war has displaced six million people, placing them at high risk of malaria infection, seeking refuge in Pakistan and Iran (5). Moreover, in Yemen, over 14.8 million people lack access to basic healthcare due to the ongoing conflict (13).
Even though Ethiopia has set a strategy for national malaria elimination, the country was affected by the COVID-19 pandemic, war, and other disasters since March 2019 and November 4, 2020, respectively. The war in Northern Ethiopia left tens of millions facing severe food insecurity and widespread infrastructure destruction. This crisis threatens immediate human survival, hinders local development, and poses significant risks to national stability (14). Hence, the Amhara region experienced service disruptions in 2021 (15).
The Amhara Region faces challenges due to the ongoing war conflict, resulting in widespread displacement. The war has severely disrupted healthcare services, forcing many health facilities to halt malaria elimination programs and essential healthcare for affected populations. This report aims to assess the patterns of malaria epidemiology and the impact of the war conflict on elimination efforts in these zones. Over the past year, eight zones have been significantly affected by the war, leading to the collapse of the healthcare system and the malaria elimination program. However, the specific impact of the war conflict on malaria elimination efforts in the Amhara Region has not been documented, and evidence remains scarce due to a lack of comprehensive evaluations. Therefore, this study aims to evaluate the effects of war on malaria in these affected areas and the overall burden in the region in 2022.
The study was conducted in Amhara National Regional State (ANRS). ANRS is one of the eleven regional states in Ethiopia. There are 22 zonal departments and 185 woreda health offices. Based on the 2007 census projections, the population of ANRS is 25, 537,286,305. The ANRS is the second most populous region. ANRS has a land mass of 154,709 km2 and lies within the geographic coordinates 11.3494° N, 37.9785° E. According to data from the Amhara Regional Health Bureau (ARHB), there were 8, 20, and 71 specialized, general, and primary hospitals, respectively, 921 health centers, and 3725 health Posts (Figure 1).
Figure 1 Map of the Amhara region by zone; war conflict-affected zones
The study was a retrospective cross-sectional design to assess the impact of war on malaria services, enabling the analysis of pre-existing data across different time points. Routine surveillance data were extracted from the archived records within the regional Public Health Emergency Management (PHEM) database. The study was conducted from 2020 to 2022.
All malaria cases within conflict-affected regions were retrieved from PHEM, focal test, and treat and foci databases. Only confirmed cases, including those diagnosed by microscopy, rapid diagnostic test (RDT), and clinically, were included in the analysis.
Due to data availability constraints, our analysis is limited to malaria case incidence rates, treatment coverage, and service availability. This information is essential for understanding the specific aspects of malaria service delivery, such as access to diagnosis, treatment, and prevention, which were affected by the conflict
To analyze the impact of the war, we compared data from pre- and post-war periods. We utilized Excel spreadsheets, Power BI, and interrupted time-series analysis with Ordinary Least Squares (OLS) to calculate relative level changes. Descriptive statistics were employed to characterize the data. After extracting the necessary data, we meticulously cleaned and formatted the dataset using Excel. To ensure data integrity, we employed record ID-based duplicate removal and data mining techniques to identify potential duplicates based on data field similarity
Ethical Approval was given by the Ethical Review Board of Amhara Public Health Institute/APHI /before accessing the secondary data. Data was only used for the study. All personal identifiers were removed from the study. The Ethical Review Board of Amhara Public Health Institution approved this study with the number NoH/R/T/T/D/5/24. To maintain data confidentiality, limit access exclusively to authorized personnel
The findings will be communicated with the responsible stakeholders, who will assist in improving the service in the form of seminars and publication in peer-reviewed journals will be considered. Additionally, the full report will be submitted to the regional health bureau, zonal health departments, woreda health offices, and supporting regional stakeholders.
Between 1994 and 2022, 185,600,714 patients received medical services in the Amhara Regional State of Ethiopia. One of the major public health issues in this region is malaria. Out of all the patients seen, 18,880,653 cases (10%) were malaria cases reported in the last 20 years. Most of these cases were detected through microscopy and Rapid Diagnostic Test (RDT), while some were reported through clinical assessments. In 2013, the malaria surveillance system was strengthened, resulting in more positive cases being confirmed through diagnostic tools (Figure 2). The number of malaria cases was alarmingly high between 2003 and 2013, but it has rapidly declined since 2014.
In the recent five-year report of weekly malaria data from 2017 to 2021, there were a total of 1,562,376 cases from which 231,034 were in 2017, 193,934 were in 2018, 363,822 were in 2019, 394,377 were in 2020 and 379,209 were in 2021. From 9,717,997 parasitological tests (Microscopy and RDT). From the total parasitological tests, microscopic diagnosis accounts for 66.1%. Of the total malaria cases, under-five children and pregnant women accounted for 12.4% and 0.9%, respectively.
The annual malaria parasite incidence/API/ of the Amhara region is higher than the national annual incidence rate in 2020; 16/1000 API at national and 18/ 1000 API, at regional. For instance, in 2020, the top five zones of API are North Gondar, Awi, South Gondar, Bahir Dar town, and Waghimra zones reported 476, 416,252,191, and 172cases per 1000 population/ Year respectively. Moreover, before the TIF disrupted the health service and destroyed the health facilities in North Wollo, South Wollo, North Shewa, Dessie town, and Oromo special zone, the annual malaria parasite incidence was 62, 26, and 43, 0.5, and 156 /1000pop/ year respectively.
Figure 2 Trend in confirmed and clinical malaria cases in Amhara region, 1994-2021 G.C
The species distribution of malaria patients also varied during two decades. About 66 % of total confirmed malaria cases were plasmodium falciparum. Then the total confirmed malaria cases declined from 1994 to 2012 year due to the high number of clinical case management present during that period (Figure 3).
Figure 3 Distribution of regional malaria confirmed malaria cases with species type from 1994 to 2020.
The regional proportion of plasmodium falciparum and test positivity rate trends indicate an increment within the last 20 years since 1994 G.C. (Figure 4)
Figure 4 Trend in malaria test positivity rate and PF proportion, Amhara Region, Ethiopia, 1994-2020
The projection of malaria cases slightly increased compared to normal situations. However, the number of malaria cases will increase due to service interruptions resulting from TIF's destruction and looting of health facilities (Figures 5-8).
Figure 5 The trend of malaria case projection
Figure 6 Trend projection of the regional malaria annual parasite incidence
Figure 7 The regional projection trend of the malaria positivity rate
Figure 8 The regional projection of the plasmodium proportion
All expected health facilities, including 3573 Health Posts, 866 Health Centers, and 82 hospitals, provided a malaria service during the pre-war period. Of these, 77 % (2751) of health posts, 79% (684) of health centers, and 78 % (63) of hospitals provided malaria service during the post-war period. This indicates that 24% of malaria services declined from pre- to post-war.
Even though the malaria services were interrupted during the post-war with the report average completeness rate of 70%, the reported cases increased from the previous year. Also, during the post-war reports of 2021 as compared to 2020 in the same week almost similar and only decreased by 1% (Figure 9).
Figure 9 Trend of malaria cases by year, Amhara region, from 2017 to 2021.
The regional malaria weekly surveillance reports decreased, below the WHO minimum requirement, during the war in affected zones. From which zones affected by war the reporting completeness was in North Wollo = 25%, Waghimra zone =18%, Dessie town=40%, South Wollo = 57%, N/Gondar=66%, and Oromo special zone 68% (Figure 10).
Figure 10 Distribution of report completeness by zone during pre-and post-war, 2021.
During post-war in the region, the malaria weekly surveillance report was interrupted for 35 weeks. Of the conflict-affected zones; malaria service of surveillance report has been interrupted in the Waghimra zone for the last 25 weeks, in the North Wollo zone for the last 24 weeks, in the South Wollo zone for the 13 weeks, and Oromia special zone for the last 10 weeks. Also, in the two months, service interruptions were reported in South Wollo zones. On the other side, the highest number of malaria cases were reported in the North Shewa Zone (Figure 11)
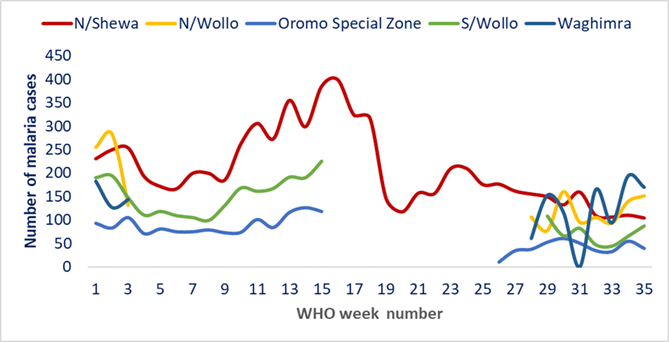
Figure 11 Trend of malaria cases by week in conflict-affected zones, 2021G.C
When we compared the pre-and post-war total malaria cases, P. falciparum and P.vivax in conflict-affected zones showed an increment in North Shewa, South Wollo, and Oromia special zone, during post-war. On the other side, the North Wollo and Waghimra zones showed a decrease as compared to the pre-war time (Figure 12).
Figure 12 Distribution of malaria cases and species type by conflict-affected zones during pre- and post-war G.C.
Distribution of malaria cases by age Group during Pre- and post-war in conflict-affected zones. Cases by age groups during the post-war period increased in the North Shewa zone and the South Wollo zone. Of the total reported under five years of age, the North Shewa zone accounted for 36% of them (Figure 13)
Figure 13 Distribution of malaria cases by age group during pre- and post-war, 2021G.C
The total number of malaria index cases investigated was higher reported in the North Shewa zone during the post-period as compared to other elimination-targeted zones. As compared to the pre-war confirmed malaria cases, in North Shewa and South Wollo malaria cases increased by 205% and 41%, respectively. Nearly seventy-four (74.1%) of malaria index cases were accounted for in the North Shewa zone during the post-period (Table 1).
Table 1 Distribution FTAT investigation report in elimination targeted zone during pre-war and post-war, 2021G.C
| Zone | North Shewa | South Wollo | North Wollo | Dessie City | ||||
|---|---|---|---|---|---|---|---|---|
| pre war | post war | pre war | post war | pre war | post war | pre war | post war | |
| Total confirmed malaria cases | 1505 | 4604 | 952 | 1351 | 551 | 296 | 24 | 35 |
| Number of index malaria cases eligible for investigation | 1212 | 3026 | 762 | 773 | 503 | 241 | 13 | 9 |
| The number of malaria index cases investigated | 1027 | 2251 | 513 | 655 | 478 | 89 | 10 | 9 |
| The number of household members tested | 18377 | 40818 | 8374 | 8481 | 7571 | 1234 | 366 | 308 |
| Total number of positive secondary cases | 125 | 200 | 53 | 52 | 124 | 26 | 0 | 0 |
A total number of confirmed malaria cases were reported during pre-war and post-war in elimination targeted zones. North Shewa zone and South Wollo zone have shown large numbers of confirmed malaria cases reported during post-war (Figure 14 and Figure 15).
Figure 14 Distribution of confirmed malaria cases in conflict-affected zones during pre-war and post-war
Figure 15 Index malaria cases investigated among eligible cases in conflict-affected zones during pre-war and post-war; 2014 vs. 2013
No active foci investigated were reported in the North Wollo zone during the post-war as compared to pre-war. In the south Wollo and North Shewa zones, more active foci were investigated during post-war (Figure 16).
Figure 16 Distribution of the total number of active foci investigated in conflict-affected zones
Most materials required for malaria elimination activities including health facilities were destroyed by the war. Materials for malaria elimination activities were distributed before the war and destroyed during the war; 100 % in North Wollo, 100% in Dessie Town, and 50% in North Shewa and South Wollo zones (Table 2).
Table 2 Destroyed material list for malaria elimination activities
| Items | Unit | # Destroyed material list |
|---|---|---|
| Hospital/Health Center OPD Malaria Registration Book | Book | 2500 |
| Focal Test and Treat (FTAT) Passive Case Documentation (Screening) Form | Book | 3000 |
| Focal Test and Treat (FTAT) Household Questionnaire | Sheet | 700000 |
| Weekly Reporting Form on Case Investigation with Reactive FTAT | Book | 2500 |
| Malaria Epidemic Monitoring Chart | Sheet | 2398 |
| Hillmen Urine Color Chart (Amharic Version) | Sheet | 963 |
| Malaria Case Management Job Aids for Hospital/Health Center | Pad | 2659 |
| Malaria Case Management Job for Health Post | Pad | 1657 |
| Microscope | Each | 360 |
Over ten million people were internally displaced and also 76 woredas and 80 kebeles were affected by war. History witnessed that IDP sites are favorable ground places for malaria transmission (Table 3)
Table 3 List of war-affected zones with a population
| Zone | # of Affected Woreda | # Affected population | # Affected Malarious Population | # Affected kebeles | # Affected Malarious Kebel |
|---|---|---|---|---|---|
| North Gondar | 6 | 877,649 | 438,086 | 6 | 6 |
| North Wollo | 13 | 1,710,538 | 1,670,903 | 13 | 13 |
| North Shewa | 8 | 818,200 | 429,150 | 12 | 12 |
| Oromia | 7 | 585,968 | 585,968 | 7 | 7 |
| South Gondar | 14 | 2,524,097 | 2,202,385 | 14 | 14 |
| South Wollo | 21 | 3,044,924 | 1,584,834 | 21 | 21 |
| Waghimra | 7 | 535,926 | 332,547 | 7 | 7 |
| Grand Total | 76 | 10,097,302 | 7,243,873 | 80 | 80 |
South Wollo and North Shewa IDP sites were a shelter for Waghimra, North Wollo, and Oromia (Wolega). South Gondar IDP site was a shelter for Waghimra and North Wollo displaced people. Bahir Dar was also flooded with thousands of IDPs coming from East Amhara and Gondar. West Gojjam and Awi Zones are still the centers of thousands of IDPs coming from Benishangul Gumuze and Oromia (Wolega). This situation is expected to increase the burden of malaria cases in zones with IDPS.
Between 2020 and 2021, armed conflicts of varying durations and intensities across the district in the region were associated with a general decrease in relative incidence ratios in conflict-affected districts, as indicated by OLS regression analysis. In the districts affected by the conflict, there is a general tendency for the relative incidence ratio to decline, according to the OLS regression analysis (Figure 17).
Figure 17 relative incidence ratio from pre to post-war Amhara Zone
Over the past 20 years, nearly all reported malaria cases have been confirmed, aligning with regional epidemiological patterns. This finding is consistent with WHO and national standards, which recommend that anyone presenting with a fever be assessed for the diagnosis and treatment of malaria (16, 17).
The regional proportion of P. falciparum trend indicates an increment. This indicator might help to assess information on the likelihood of observing severe cases and provides information on the degree of malaria control, as, in areas where control measures are scaled up, the proportion of cases due to P. falciparum may decrease.
The regional test positivity rate is usually computed for a specific period of case detection activities. It has declined even if not filled by the national malaria elimination program for shifting the control phase into the pre-elimination phase, which is less than a 5% test positivity rate. It might indicate that not all febrile cases were screened for malaria (16).
During the war, we analyzed data on malaria transmission to clarify the effect of conflicts on the disease incidence. The results of the current study can provide a new outlook on malaria elimination program planning not only in targeted zones but also in all zones in the region. Malaria risk was found to be dependent on population situation and movement (18). As estimated, during unstable social conditions during the conflict, a relatively high malaria infection rate was observed among under five and from five to fourteen age groups. This may indicate that the exposure of people to mosquito bites was relatively high due to the unfavorable situation of their IDP sites. (Figure 13).
The regional malaria elimination program during the war was interrupted; in the elimination program, a single case has an impact on onward transmission. These conditions may increase malaria transmission and lower-case detection and notification. This report also significantly indicates war-caused national elimination programs in targeted zones and non-invaded areas set goal interruption (Figure 11).
The current war in Ethiopia exponentiated the burden of malaria infection, transmission, and complications due to the destruction of health facilities and looting of medical equipment and supplies including Anti-malaria drugs, supplies and internal displacement. Malaria patients were left without any care and they were forced to flee where IDP centers were found. This could have resulted in a rapid increase in morbidity and mortality of malaria among populations most severely affected by war and IDP centers including catchment populations (19).
Malaria epidemic during the war, ancient evidence confirmed that wars had an evolutionary impact on malaria transmission burden. War devastated the malaria prevention, control, and elimination programs and resulted in forced displacement of malaria transmission conflict affecting others. An increase in vectorial capacity due to the high production of vector anopheline mosquitoes was probably critical. This could have resulted from more breeding places (or deterioration in larval control), prolonged mosquito survival, or increased man-vector contact (19, Figure 9).
Evidence shows that there is a risk of exacerbation P. falciparum species during an ongoing war, and our analysis revealed the likelihood of a malaria outbreak due to the magnitude of P. Falciparum is responsible for the majority of malaria deaths globally and is the most prevalent species in sub-Saharan Africa. Similar findings were reported in irregular migrants who returned to Sri Lanka from West Africa (20).
Cases of malaria and foci notification, investigation, and response have been greatly impacted by war in the Amhara region of Ethiopia. The finding shows that there has been a gradual increase in malaria transmission rates in IDP centers and surrounding locations, with late detection and response in war-affected areas. During the post-war period, the majority of cases were reported in the North Shewa zone and South Wollo zone, possibly due to the migration of people from nearby zones and IDP collection sites. Similar reports have shown that wars, social conflict, and migration have been significant factors contributing to the increased risk of malaria in some Asian countries and the Dezful district, which experienced two wars (5).
There is no uncertainty that the consequence of population movement on malaria is widely treated as infected people who move into malaria-free or low areas may introduce the parasite into different areas, particularly those that have appropriate vectors. There is no uncertainty that the movement of people can significantly impact malaria. When infected individuals move to malaria-free or low-risk areas, they can potentially introduce the parasites to new areas, especially those that have appropriate vectors (21). All forced displaced populations are not commonly reached by government malaria elimination programs in conflict-affected areas. Most research findings indicated efforts are based on treating human groups as stable entities and do not account for possible mobility (22). Therefore, displaced populations drop out of the loop of most public health efforts since difficult to manage in IDP sites and temporary homes often cannot be identified and therefore, do not receive services.
However, the area is earmarked for malaria elimination, but the presence of illegal migrants with their treatment-seeking behaviour confounds anti-malaria operations. Thus, such as the use of bed nets, access to antimalarial drugs, and health education may be vital for reducing risk in the reported area.
It has been found that various government malaria elimination programs in conflict-affected areas are unable to reach all forced-displaced populations. This is because such efforts are mostly based on treating human groups as stable entities, without considering their potential mobility. As a result, displaced populations often miss out on most public health efforts, as they are difficult to manage in IDP sites and temporary homes that cannot be identified for providing services. Despite being earmarked for malaria elimination, the presence of migrants and their treatment-seeking behavior complicates anti-malaria operations in the area. Therefore, it is important to provide access to antimalarial drugs, health education, and the use of bed nets to reduce the risk in the reported area.
According to a series of analyses of interrupted time, the incidence ratio in areas affected by conflicts has generally decreased from pre-war to post-war, despite an increase in the number of cases since the start of the conflict. This shift may be due to lower case detection rates caused by operational flaws in the monitoring system or a decline in treatment-seeking behavior in those areas, given the overall higher rate of malaria. A weak surveillance system may result in inadequate case management and vector control strategies (23). Due to the violence, malaria diagnosis and treatment became less accessible, and there was significant damage to health facilities and medical equipment looting (24, 25).
Malaria is a major public health concern in the Amhara region, and it contributes to the majority of cases in the country. Late detection and underdiagnosed malaria cases are more prevalent. The war led to malaria transmission, reactivation, and failure of malaria elimination in both Tigray Invading Force-affected and unaffected zones. The regional malaria elimination program in focal test and treatment and foci investigation has been hindered. Vigilance surveillance in malaria elimination programs is mandatory for screening, active case finding, and effective management. Developing guiding documents for the anti-malarial modality for mobile health teams and internally displaced persons (IDPs) is crucial. It is also vital to strengthen the engagement of all stakeholders to continue the elimination efforts and fill in gaps left by the conflict. Epidemiological studies must be conducted to monitor the transmission dynamics.
We appreciate the Amhara Public Health Institute for granting us access to the relevant data for this study.
API-----Annual Malaria Parasite Incidence
ANRS-----Amhara National Regional State
ARHB----Amhara Regional Health Bureau
FTAT-----Focal test and treat
IDP-----Internal Displaced Person
HC -----Cener
HP-----Health Post
OLS-----Ordinary Least Squares
NMEP---National Malaria Elimination Program
PHEM---Public Health Emergency Management
RDT-----Rapid diagnostic test
WHO---World Health Organization
Ethical clearance was obtained from the Amhara Public Health Institute (NoH/R/T/T/D/5/24)
Not applicable.
Data are available upon reasonable request.
The authors declare no competing interests.
This study did not receive any specific grants from funding agencies in the public, commercial, or not-for-profit sectors.
Mastewal Worku wrote the manuscript by analyzing and interpreting the data. The manuscript was edited and contributed to by each co-author.