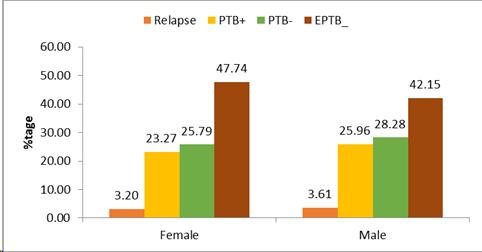
Figure 1 Distribution of Type of TB by Sex
War and its implications for the tuberculosis program in the Amhara Region
1Amhara Public Health Institute, Bahir Dar, Ethiopia
2School of Public Health, College of Medicine and Health Sciences, Bahir Dar University, Bahir Dar Ethiopia
3Department of Health Systems and Policy, Institute of Public Health, College of Medicine and Health Sciences, University of Gondar, Gondar, Ethiopia
*Corresponding Author: Melashu Balew, Email: bmelashu@gmail.com Bahir Dar, Ethiopia,
Background: War is one of the most significant factors exacerbating tuberculosis (TB) epidemics, increasing both morbidity and mortality rates. Direct attacks on healthcare facilities and medics, displacement of millions of people, and challenges with access to and delivery of medicines disrupt patients' treatment. This study aimed to assess war and its implications for the TB control program in the Amhara region.
Methods: Retrospective data archived in the regional Health Management Information System (HMIS) database were extracted to understand the regional TB program in the prewar period and forecast the impact of war on the TB control program. Four years of secondary archived data (July 2019 to December 2022.) were used to forecast TB incidence and treatment outcomes in war-affected zones in 2022. To validate the model, the results were compared with actual observed TB incidence data. Line graphs and bar charts were used to compare the incidence of TB across age and sex categories.
Results: The TB incidence rate in North Wollo, Waghimira, and North Gondar (war-affected zones) was 198.7, 169.7, and 142 per 100,000, respectively. Among females, the proportion of extrapulmonary TB (EPTB), clinically confirmed TB cases, and pulmonary TB cases were 49.3%, 26.6%, and 24.0%, respectively. In the region, 204 drug-resistant TB cases were notified. TB patients, including those with multidrug-resistant TB (MDR-TB), were left without care and were forced to flee to internally displaced persons (IDP) centers. Of the 116 drug-susceptible TB patients identified during the war, 85 (73.3%) were from IDP sites. According to the six months HMIS report, Zones had zero TB case notification. The TB control program was interrupted for nine months in war-affected zones and severely attenuated in other zones.
Conclusion: The incidence of TB in war-affected areas was high. Severe types of TB and under-diagnosed cases were more prevalent, which could lead to high TB transmission, reactivation, and drug resistance development in both war-affected and non-affected zones. Therefore, strengthening active and passive case finding, restoring diagnostic capacity, providing Bacillus Calmette-Guérin (BCG) vaccination, conducting rigorous TB screening and surveillance, and managing TB, including severe forms such as MDR-TB and Extensively drug-resistant tuberculosis (XDR-TB), are crucial measures to enhance the regional TB control program.
Keywords: War, TB, implication, Amhara.
የጥናቱ ዳራ፡- የቲቢ በሽታ ወረርሽኝን ከሚያባብሱ በጣም አሳሳቢ መንስኤዎች አንዱ ጦርነት ነው። ጦርነት በቲቢ ምክያት የሚመጣ የበሽታ መከሰትና ሞት መጠንን በእጅጉ ያባብሳል። በጤና ተቋማትና ሠራተኞች ላይ በሚደርስ ቀጥተኛ ጥቃት እንዲሁም የሚሊዮኖች መፈናቀልና በመድኀኒት አቅርቦትና ተደራሽነት ላይ በሚፈጠሩ ችግሮች የታማሚዎች ህክምና ይስተጓጐላል። ይህ ጥናት ዓላማ አድርጎ የተነሳው ጦርነቱ በአማራ ክልል የቲቢ በሽታ ቁጥጥር መርሐግብር ላይ ያደረሰውን ተፅዕኖ መመርመርና በክልሉ ያሉ ችግሮችን ለመቅረፍ ሳይንሳዊ ይሁንታዎችን መጠቆም ነው።
የጥናቱ ዘዴ፡- በቅድመ ጦርነት ወቅት የነበረውን የአማራ ክልል የቲቢ በሽታ ቊጥጥር መርሐግብር ለመገንዘብና ጦርነቱ በቲቢ በሽታ ቊጥጥር መርሐግብር ላይ ያሳደረውን ተፅዕኖ ለመተንበይ ከክልሉ የጤና አስተዳደር መረጃ ሥርዓት (HMIS) የመረጃ ቋት ውስጥ የኋላ ታሪክ መረጃ ተወስዷል። በዚህም እ.አ.አ. በ2022 በጦርነት የተጐዱ ዞኖች ውስጥ የቲቢ በሽታ መከሰትና የተሰጡ ህክምናዎችን ውጤቶች ለመተበንይ የአራት ዓመታት (ከሐምሌ 2012 አስከ ታኅሳስ 2014 ዓ.ም) ዳኅራይ የሰነድ መረጃዎች ጥቅም ላይ ውለዋል። ሞዴሉን ለማረጋገጥ ደግሞ የሞዴሊንግ ውጤቱ ከታየው ትክክለኛ የቲቢ በሽታ ክስተት መረጃ ጋር በንጽጽር ቀርቧል። በተጨማም የቲቢ በሽታ ክስተት በጾታና በእድሜ ምድቦች ላይ ያለውን ስርጭት ለማነጻጸር የመስመር ግራፎችና የባር ቻርቶች ጥቅም ላይ ውለዋል።
የጥናቱ ውጤት፡- በጦርነቱ በተጐዱ ሰሜን ወሎ፣ ዋግ ኽምራና ሰሜን ጎንደር ዞኖች የቲቢ በሽታ መከሰት መጠን ከ100000 ሰዎች መካከል በቅደም ተከተል 198.7፣ 169.7 እና 142 ነው። ከሳንባ ውጭ ያሉ አካላትን የሚያጠቃ ቲቢ በሽታ መከሰቶች፣ በህክምና የተረጋገጡ የቲቢ በሽታ መከሰቶች፣ እና ሳንባን የሚያጠቃ የቲቢ በሽታ መከሰቶች በሴቶች መካከል ያላቸው ስርጭት በቅደም ተከተል 49.3 በመቶ፣ 26.6 በመቶ እና 24 በመቶ ነበር። በክልሉ ውስጥ 204 መድኅኒት የተላመደ የቲቢ በሽታ ተጠቂዎች ተመዝግበዋል። ብዙ መድኀኒቶችን የተላመደ የቲቢ በሽታ ታማሚዎችን ጨምሮ እነዚያ በሽተኞች ያለምንም ክትትልና ጥንቃቄ ተትተዋል፤ የሀገር ውስጥ ተፈናቃዮች ወደ ሚገኙባቸው መጠለያ ጣቢያዎች እንዲሸሹ ተገድደዋል። በጦርነቱ ወቅት ከተለዩ 116 ለመድኀኒት መላመድ ተጋላጭ የሆኑ የቲቢ በሽታ ታማሚዎች ውስጥ 85 (73.3 በመቶ) ታማሚዎች ከሀገር ውስጥ ተፈናቃዮች መጠለያ ጣቢያዎች የተለዩ ናቸው። በስድስት ወሩ የጤና አስተዳደር መረጃ ሥርዓት ዘገባ መሠረት በህወሓት ከተወረሩ ዞኖች ውስጥ ምንም የቲቢ በሽታ መከሰቶች አልተገለጸም። የቲቢ በሽታ ቊጥጥር መርሐግብር በጦርነት በተጎዱ አካባቢዎች ለ9 ወራት ተቋርጦ የነበረ ሲሆን በሌሎች አካባቢዎች ደግሞ እጅግ በጣም ተዳክሞ ነበር።
የጥናቱ ማጠቃለያ፡- በጦርነቱ በተጎዱ አካባቢዎች የቲቢ በሽታ መከሰቱ ከፍተኛ ነበር። ለከፍተኛ የቲቢ ስርጭት፣ ማገርሸትና የመድኀኒት መላመድ እድገቶች የሚዳርጉ ከባድ የቲቢ በሽታ ዓይነቶችና ያልተመረመሩ ህመሞች በጦርነቱ በተጐዱም ሆነ ባልተጐዱም በሁለቱም አካባቢዎች በጣም ተስፋፍተው ነበር። ስለዚህ አዲስ ህመምተኞችና ታመው የነበሩን መለየት ማጠናከር፣ መልሶግንባታ፣ የቲቢ ክባት ማቅረብ፣ ጠንካራ የቲቢ ታማሚዎች ልየታና ቅኝት፣ እና ብዙ መድኀኒት የተላመደ ቲቢን (MDR-TB)ና ሁለተኛ ደረጃ ላይ ያሉ መድኀኒቶችን የተላመደ ቲቢ (XDR-TB) ጨምሮ ከባድ የቲቢ በሽታ ዓይነቶችን ማስተዳደር ክልላዊ የቲቢ በሽታ ቊጥጥር መርሐግብርን ለማሳደግ ሊተገበሩ የሚገባቸው ርምጃዎች ናቸው።
ቁልፍ ቃላት፡- ጦርነት፣ ቲቢ፣ መከሰት፣ የህክምና ውጤት፣ አማራ
War and armed conflicts have both direct and indirect effects on public health. They deteriorate the health of the population by causing the breakdown of the healthcare system, creating shortages of medical supplies, and leading to the relocation of healthcare personnel. Additionally, conflicts disrupt food and clean water sources1. Tuberculosis remains a major cause of morbidity and mortality. According to the World Health Organization (WHO) 2020 report, the global TB incidence was 127 per 100,000, and TB-HIV mortality was 214,000 2. TB is one of the world’s main health challenges, with 10 million new cases and nearly 1.5 million deaths each year 3. Due to the COVID-19 pandemic, there was a sharp decrease in TB detection by 18%, from 7.1 million cases in 2019 to 5.8 million cases in 2020. In the 2020 COVID-19 era, TB ranked as the 13th leading cause of death and the second leading infectious killer after COVID-192.
In Ethiopia, one of the 30 high TB burden countries, the incidence of TB was 132/100000. Specifically, TB/HIV co-infection rate reached to plateau of 26.7% in Amhara National Regional State (ANRS) 4. The treatment success rates for first and second-line TB treatment were 90% and 70%, respectively2. The sudden attack by the Tigraian invading force, known as Mebrekawi Tikat, on the Ethiopian national army stationed in Tigray, precipitated a new war that forced the displacement of the Amhara people. As a result, health facilities were purposefully destroyed. These conditions significantly increase the risk of infectious diseases such as tuberculosis among people living in war-affected areas and those displaced from their villages5.
TB is one of the most frequent and most dangerous diseases that is further complicated by war. It was a major health disaster during World War II. As has been seen, the longer and more widespread a war, the greater the increase in tuberculosis cases 6,7. In war zones, the treatment of TB patients is disrupted by direct attacks on healthcare facilities and medical personnel, as well as by the displacement of millions of people and challenges in accessing and delivering medicines 8.
During emergencies such as conflict-related humanitarian crises and migration crises, delivering public health services to meet the healthcare needs of affected populations becomes extremely challenging. While relocation to camps or other temporary settlements is a common solution after displacement, it can exacerbate vulnerability to TB due to overcrowding, malnutrition, disruption of regular healthcare services, poor health-seeking behavior, and inadequate adherence to TB treatment medications 9.
During emergencies, the collapse of health systems reduces access to TB awareness, prevention, and continuous care at origin points, during transit, at destinations, and upon return across borders. Addressing critical concerns includes limited TB case identification, inadequate TB services, drug supply interruptions, irregular drug intake, increased treatment defaults, low cure rates, higher rates of patient relapse, and the rise of Multidrug-resistant (MDR) TB, among other challenges 10,11.
Before the war, the treatment success rates for first- and second-line TB treatment were 90% and 70%, respectively, in the Amhara region. However, the region has been severely affected by the war for over a year, with eight zones invaded and people displaced from their homes by the TIF. In this war zone, the healthcare system collapsed, leaving TB patients without access to anti-TB drugs. As a result, these patients not only had to interrupt their medication but also became potential sources of TB infection to others, contributing to the rapid spread of TB, including drug-resistant strains. This situation poses a critical public health problem. However, the impact of the war on tuberculosis in the Amhara region has not been documented, and evidence is limited. Thus, this study aims to determine the effect of the war on TB in affected areas and the overall burden in the region.
The study was conducted in the Amhara National Regional State (ANRS) with a special emphasis on war-affected areas. ANRS is one of the eleven regional states in Ethiopia. The regional state comprises 22 zones and 216 woredas. ANRS is the second most populous region in Ethiopia. Based on 2022 projections, the population of ANRS is 22,286,999, with 11,400,762 males and 11,476,236 females. ANRS covers a land area of 154,709 km² and is located at the geographic coordinates 11.3494° N, 37.9785° E.
The region has 110 hospitals (100 Public and 10 private). Among the public hospitals, 8 are comprehensive specialized hospitals, 13 are general hospitals, and 65 are primary hospitals. Additionally, there are 874 public health centers, 3,561 health posts, and over 1,300 other private health facilities. However, 5 (31%) zonal health departments, 52 (24%) district health offices, 40 (41%) public hospitals, 453 (49.4%) health centers, and 1,850 (49.7%) health posts were destroyed to varying extents by the TIF. This destruction severely impacted service provision as well as the TB detection and control system.
A cross-sectional study design was employed to determine the effect of war on TB in war-affected areas. The study was conducted from March 1-31, 2022, using secondary data archived from July 2019 to December 2021 for projection, and primary data collected from December 24, 2021, to January 14, 2022, from war-affected health facilities for comparison with actual TB incidence cases.
All TB-screened patients in the war-affected areas of the Amhara region
All screened patients in the war-affected areas of the Amhara region were included in this study. However, patients with incomplete secondary data records were excluded.
Eight war affected zones (North Wollo, South Wollo, North Shewa, Dessie City Administration, South Gondar, Waghimra, North Gondar and Oromo special zones) and one hundred thirteen accessible health facilities in the war-affected zones were recruited by purposive sampling.
Both primary and secondary data were collected from recruited zones and health facilities. All TB cases registered in Health Management Information System/District Health Information Software 2 (HMIS/DHS2) and LIS, including rifampicin resistance (RR)/MDR-TB and treatment outcomes, were described in the study. The national and regional TB programs are supported by various laboratory techniques, including solid and liquid culture, line probe assays, Expert MTB/RIF assays, fluorescence microscopy, and Ziehl-Neelsen (ZN) microscopy. TB patients were classified as bacteriologically confirmed Pulmonary TB (PTB+), clinically diagnosed PTB (PTB-), and extrapulmonary TB (EPTB). A bacteriologically confirmed PTB case refers to a patient from whom at least one biological specimen is positive for MTB by smear microscopy, Xpert MTB/RIF, or culture. A clinically diagnosed TB case refers to a patient who does not meet the criteria for a bacteriologically confirmed case but has been diagnosed with active TB by an experienced clinician and has been determined to require a full course of TB treatment 12. EPTB refers to any bacteriologically confirmed or clinically diagnosed case of TB involving organs other than the lungs. Diagnosis should be based on at least one specimen with confirmed MTB or histological or strong clinical evidence consistent with active EPTB, followed by a decision by a clinician to treat with a full course of TB chemotherapy. Patients with rifampicin resistance defined as RR-TB cases 12. The study included a rapid assessment during the pre- and post-war periods to evaluate the trends of TB and its types over time. Additionally, the total TB data were analyzed by disaggregating them according to age and gender.
The HMIS system is currently well-integrated and utilized health information reporting and archiving system in Ethiopia. The HMIS system is a well-integrated and widely utilized health information reporting and archiving system in Ethiopia. Data quality assurance is conducted at both the facility and woreda (district) levels. Lot quality assurance sampling (LQAS) methods are employed on a monthly basis at the facility level and quarterly at the woreda level to ensure high standards of data quality 12. Moreover, the quality of TB data in the Directly Observed Therapy Shortcourse (DOTS) program is maintained through continuous training and supportive supervision. Taken together, several lines of measures were in place to maintain data quality and avoid systematic bias.
All TB cases were retrieved from HMIS/DHIS2 and LIS databases and included in the analysis. Additionally, a rapid assessment was conducted at 113 health facilities to evaluate their status before and after the war.
Authors had full access to the HMIS database. After transferring the required data from the database to the new Excel sheet, data owners cleaned and formatted the imported dataset. This included converting numbers stored as text into numbers, removing duplicate, spacing, merging lines and deleting unnecessary variables. The study included zonal level data archived in a single HMIS database classified with reporting period. Separate Excel datasets from four years were merged using the consolidate data wizard.
The data were analyzed using Excel spreadsheets. Descriptive statistics were employed to characterize based types of data. Trend analysis and forecasting of tuberculosis were conducted using linear and poly models. Additionally, choropleth mapping was utilized to visualize the TB burden across zones using ArcGIS 3.4. Spatial data for the maps were sourced from the Map Library, a public domain accessible at www.maplibrary.org. Finally, the data were presented using proportions, line graphs, and bar graphs.
In war affected areas, 111,056 TB cases were notified from July 2011 to 2014 E.C. The cases were detected by microscopically, GenXpert, culture and clinically. There was a total of 141569 TB cases in 3 years period from which 50444 cases were in 2011 E.C, 47354 cases were in 2012 E.C, and 43771 TB cases were in 2013 E.C. Those cases notified in 2013 E.C were from West Gojjam (4594 cases), South Wollo (4530 cases) and Central Gondar (4202 cases).
According to the annual TB reports submitted to HMIS/DHIS2 and LIS, a total of 111,056 TB cases were notified from July 2019 to 2022. These cases were detected using microscopy, GenXpert, culture, and clinical methods. Over a three-year period, there were a total of 141,569 TB cases, with 50,444 cases reported in 2019, 47,354 cases in 2020, and 43,771 cases in 2021. Specifically, in 2021., significant numbers of cases were reported from West Gojjam (4,594 cases), South Wollo (4,530 cases), and Central Gondar (4,202 cases) (Table 1).
Table 1 Tuberculosis incidence and types of TB, Amhara region, 2021
| Zones | Pulmonary positive TB | Pulmonary Negative TB | EPTB | Relapse | Total | Incidence/100,000 pop. |
|---|---|---|---|---|---|---|
| Awi | 490 | 706 | 1330 | 42 | 2568 | 194.1 |
| Bahir Dar City | 175 | 237 | 532 | 27 | 971 | 249.5 |
| Central Gondar | 1172 | 1050 | 1846 | 134 | 4202 | 184.4 |
| Dessie City | 76 | 128 | 203 | 15 | 422 | 154.4 |
| East Gojjam | 1096 | 942 | 1934 | 66 | 4038 | 147.3 |
| Gondar City | 190 | 187 | 287 | 46 | 710 | 164.3 |
| North Gondar | 396 | 268 | 550 | 66 | 1280 | 142.1 |
| North Shewa | 1082 | 1070 | 735 | 178 | 3065 | 131.3 |
| North Wollo | 740 | 772 | 1434 | 90 | 3036 | 169.7 |
| Oromo Special | 362 | 348 | 444 | 66 | 1220 | 206.2 |
| South Gondar | 674 | 1084 | 2088 | 108 | 3954 | 151.1 |
| South Wollo | 1168 | 1172 | 2082 | 108 | 4530 | 146.3 |
| Waghimera | 152 | 454 | 462 | 50 | 1118 | 198.7 |
| West Gojjam | 814 | 1028 | 2620 | 132 | 4594 | 166.5 |
| West Gondar | 486 | 314 | 746 | 58 | 1604 | 357.4 |
In 2021, West Gondar, Bahir Dar, and Oromia Special Zones reported TB incidence rates of 357.4, 249, and 206.2 cases per 100,000 population, respectively. Before the Tigray invading force (TIF) disrupted health services and destroyed health facilities in North Wollo, Waghimira, and North Gondar, the TB incidence rates were 198.7, 169.7, and 142 per 100,000 population, respectively (Table 1).
Over the past 7 years, Rifampin Resistant (RR) TB was detected in 1,178 cases (5.04%) out of 321,568 clients tested using GenXpert. The utilization of Xpert was reported in 4 years, with the highest utilization rate observed in 2018 (88.6%) and the lowest in 2020. (45%) (Table 2).
Table 2 Tuberculosis and rifampicin resistance detection, Amhara region, 2015-2022
| Indicators | Year | |||||||
|---|---|---|---|---|---|---|---|---|
| 2015 | 2016 | 2017 | 2018 | 2019 | 2020 | 2021 | 2022 | |
| N (%) | N (%) | N (%) | N (%) | N (%) | N (%) | N (%) | N (%) | |
| Number of Xpert sites | 14 | 18 | 23 | 24 | 55 | 55 | 53 | 50 |
| Number of Xpert tests | 7208 | 16018 | 25579 | 56246 | 61864 | 55769 | 66382 | 32502 |
| Number of MTB+ identified | 1022 (14.2) | 1690 (10.6) | 1952 (7.6) | 3777 (6.7) | 4037(6.5) | 3740(6.7) | 4859 (7.3) | 2282(7.0) |
| Number of RR+ identified | 118 (11.5) | 133 (7.9) | 127(6.5) | 154(4.1) | 192(7.8) | 184(4.9) | 198(4.1) | 72(3.2) |
| Number of Indeterminate results, | 46(0.6) | 65(0.4) | 30(0.1) | 46(0.1) | 61(0.1) | 55(0.1) | 126 (0.2) | 61 (0.2) |
| Number of unsuccessful tests | 747(10.4) | 1195(7.5) | 1950(7.6) | 4024(7.2) | 3379(5.5) | 3540(6.4) | 4257(6.6) | 2328(7.2) |
| - With Error | 234(31.3) | 618(51.7) | 757(38.8) | 2188(54.4) | 1731(51.2) | 1933(54.6) | 2578(60. 6) | 1168(50.2) |
| - With Invalid | 334(44.7) | 473(39.6) | 766(39.3) | 1003(24.9) | 238(7.0) | 208(5.9) | 203(4.8) | 76(3.3) |
| - With No result | 179(24.0) | 104(8.7) | 427(21. 9) | 833(20.7) | 1380 (40.8) | 1399(39.5) | 1476(37.7) | 1054(45.3) |
| Utilization rate (%) | No data | No data | 67.6 | 88.6 | No data | 45 | 54.52 | 49.42 |
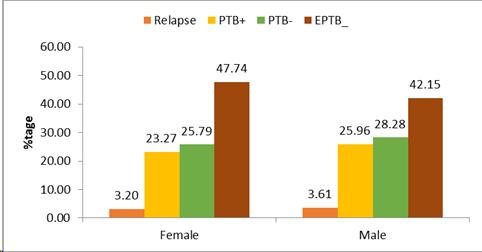
The severe form of TB disproportionately affects women and children in the region. Among females, the proportion of EPTB cases was 49.32%, followed by clinically confirmed TB cases (Pulmonary negative) at 26.64% and bacteriologically confirmed TB cases (P_POS) at 24.04%. Similarly, among males, the proportion of EPTB cases was 43.72%, with pulmonary negative and Pulmonary positive cases at 29.34% and 26.93%, respectively. Across all zones, there is an increasing trend in TB cases among males for all types of TB. Regionally, males were affected more than females by 0.6%, 2.0%, and 4.2% for pulmonary positive, pulmonary negative and extrapulmonary tuberculosis, respectively. The relapse rate was also 4.2% higher in males compared to females in the region. The distribution of TB types varies across age groups and by gender (Figure 1 and Figure 2).
In the prewar period, 204 drug resistant TB cases were notified in the region. However, reports on TB case detection and treatment outcomes were missed in war conflict areas because of the TB care service was completely disrupted, medicines including anti-TB drugs were looted, the population including TB patients and healthcare providers who had worked in TB clinic were displaced. In this humanitarian challenging situation, not only unable to screen new incidence cases, but also TB patients who were on anti-TB treatment were forced to interrupt their medication. Moreover, due to this protracted conflict, millions including new cases and interrupters aggregated in different internal displacement (IDP) centers.
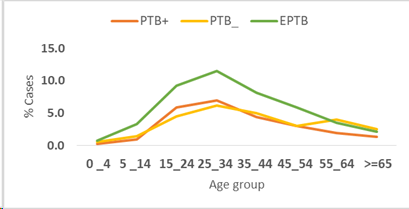
It was anticipated that TB patients in TIF-occupied zones, who were displaced to other areas, would seek and be connected to alternative TB care sites. Additionally, an increase in TB incidence was expected in IDP areas due to displacement and new notifications. However, upon comparing the half-year TB reports from non-invaded areas, TB case notifications remained unchanged, and in some zones, there was even a decrease in notifications (Figure 3).
In war-affected zones, TB notifications were either absent or decreased by half. This indicates that the impact of the war extended beyond zones directly affected by TIF, severely affecting the TB programs in other zones of the Amhara region. Additionally, 4,806 TB patients were unable to access their treatment, among whom four cases were diagnosed with multidrug-resistant TB and defaulted on their treatment, posing a significant safety risk to the community.
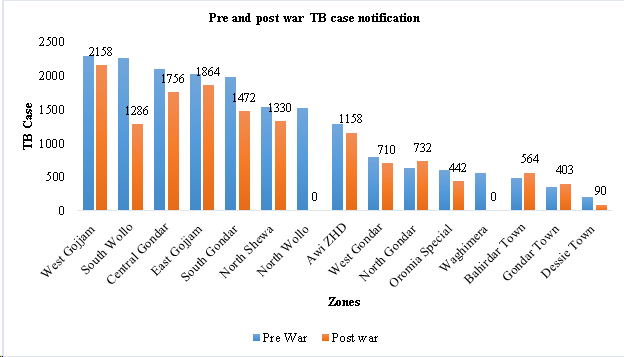
Based on the 2021 annual TB report, the incidence of TB in the post-war period was estimated for the war-affected zones. Initially, the projection indicated a slight increase in TB cases under normal circumstances. However, due to the destruction and looting of health centers, health posts, and hospitals by TIF, services were interrupted for more than six months, with potential exacerbation in areas where conflict persisted. After factoring in these conditions, the projected number of TB cases was expected to triple. In 2021, assuming normal conditions, the total TB notifications were projected as follows in the war-affected zones: 7,065 in North Gondar, 2,962 in South Wollo, 3,711 in North Wollo, 1,474 in Oromo special zone, 1,543 in Waghimra, and 392 in Dessie town (Figure 4).
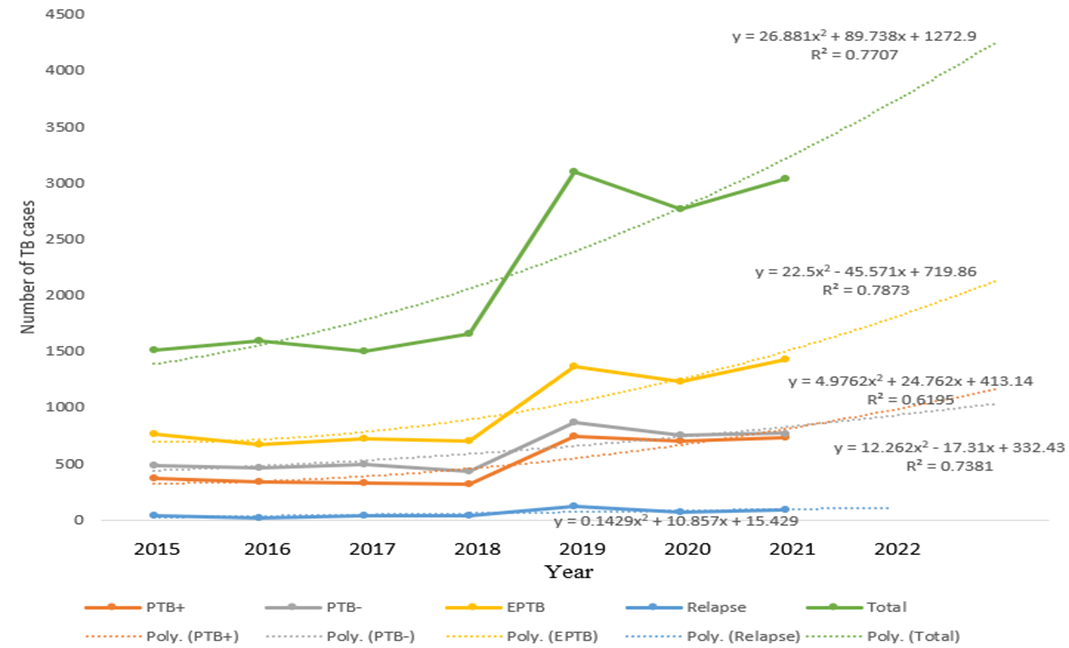
For instance, in North Gondar, one of the war-affected areas there was a decreasing trend in TB cases from 2015 to 2018, except for TB relapse cases which showed consistent numbers. However, from 2019 to 2021, there was a slight increment in TB cases. The projection for extra-pulmonary tuberculosis (EPTB) cases was 550 in 2021, but it was estimated to increase from 396 in 2021 to 1,360 in 2022. Similarly, PTB positive and PTB negative cases were projected to increase from 396 and 268 in 2021 to 756 and 835 in 2022, respectively. Overall, the trend in TB case notifications showed a sharp decrement from 2018 to 2019 and an increasing tendency from 2020 to 2021. The estimated total number of all forms of TB case notifications for 2022 is 1,270. However, despite projections showing an increasing trend since 2020, actual case detection is expected to decrease due to internal displacement, lack of access to health services, and interruptions in service delivery (such as inability to access anti-TB drugs, lack of screening and diagnosis services) in conflict areas.
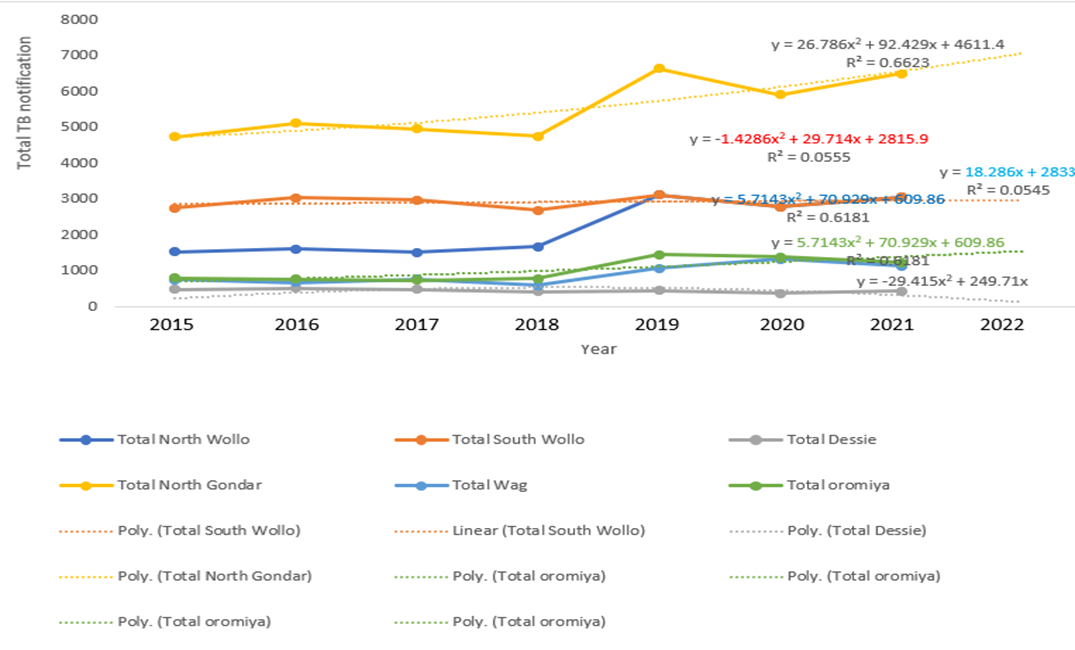
North Wollo, one of the highly affected zones in ANRS due to war, showed stable TB case detections from 2015 to 2018, except for relapse TB cases. There was a rapid increase from 2018 to 2019 in all forms of TB, followed by a decreasing trend from 2019 to 2020. A one-year projection indicates that all forms of TB case notifications were expected to increase, except for relapse TB cases. However, due to internal displacement, overcrowding, hunger, and the absence of TB preventive and control measures in war-affected zones, the number of TB infections was projected to triple or quadruple. Despite our estimations suggesting an increase in TB case detection in all forms of TB in 2022 the destruction of health infrastructure, looting of laboratory materials, medical equipment, and imaging materials, as well as the cessation of services for months, led to a significant decline in TB case detection rates, approaching zero (Figure 5).
Over 5 million people were internally displaced in the region. The South Gondar IDP site sheltered displaced people from Wag Hemra and North Wollo. Bahir Dar also saw an influx of thousands of IDPs from East Amhara and Gondar. West Gojam and Awi Zones continue to host thousands of IDPs from Benishangul Gumuze and Oromia (Wollega). This situation is expected to increase the number of new TB cases in zones with IDPs. The environment in the IDP sites and the war-affected community was conducive to TB outbreaks. Of the 116 drug-susceptible TB patients identified, 85 (73.3%) were from IDP sites. The number of known drug resistant TB patients who had their treatment interrupted and then traced back for continued /restarted treatment/ or declared outcomes, was 8 in the IDP sites and 43 in the war-affected community (Table 3).
Table 3 Number of TBL/ DR TB Cases identified in IDPs and war affected community, Amhara region March 2022
| Indicators | IDPs (collective/Host community) | War affected community | Total |
|---|---|---|---|
| Number of drug susceptible TB patients newly identified & started treatment | 85 | 31 | 116 |
| Number of known drug susceptible TB patients interrupted and trace back for continued / restarted treatment / declared out come | 350 | 1387 | 1737 |
| Number of Newly identified drug resistance TB (DRTB) linked to TIC & started treatment | 5 | 2 | 7 |
| Number of known drug resistant TB Patients interrupted and trace back for continued /restarted treatment/ declared out come | 8 | 43 | 51 |
| Number of leprosy pts newly identified & started treatment | 9 | 0 | 9 |
| Number of known Leprosy pts interrupted and trace back for continued / restarted treatment/ declared outcome | 17 | 165 | 182 |
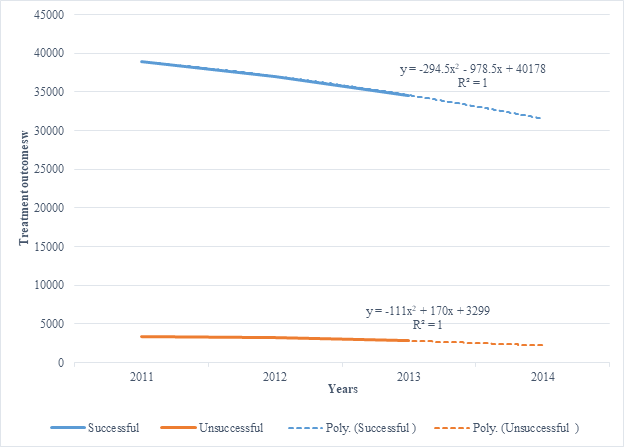
TB treatment outcomes can be classified as treatment success (cure and completed), relapse, failure, death, loss to follow-up, move to drug resistance (DR), not evaluated, and unknown treatment outcome. In general, treatment outcomes have slightly decreased over the last three years. Treatment success rates were 38,905 in 2019, 37,043 in 2020, and 34,592 in 2021. Similarly, relapsing cases showed a slight decrease from 1,394 in 2019 to 1,180 in 2021 The total deaths over three consecutive years remained similar: 1,115 in 2019 and 2020, and 1,019 in 2021. According to 2022 predictions, treatment success did not significantly change. However, due to the distraction of health facilities and the looting of anti-TB drugs, patients may not complete their treatment. The treatment success rate is expected to drop significantly, and relapsed TB cases are likely to increase dramatically. With internal displacement, there will be poor treatment adherence, increased loss to follow-up, treatment failure, and relapsed TB cases. Additionally, TB-related complications, deaths, and the transition to MDR-TB will increase exponentially due to service interruptions (Figure 6).
In this study, the incidence of TB in almost all zones of the Amhara region is much higher than the national TB incidence rate of 132 per 100,000 2. This could exponentially increase the burden of TB infection, transmission, and complications in the Amhara region, where the destruction of health facilities, looting of medical equipment and supplies including anti-TB drugs, and frequent internal displacement occur. The present study also pointed out that TB patients, including those with MDR-TB, were left without any care and forced to flee to IDP centers. This could have resulted in a rapid increase in morbidity and mortality from tuberculosis, including augmented transmission among populations most severely affected by the war and in IDP centers, as well as the surrounding populations 13. Similarly, autopsy, imaging, and molecular evidence showed that among people who died due to war-related displacement and battles, there was a high incidence of pulmonary tuberculosis 14.
In the region, 204 drug-resistant TB cases were reported. As stated earlier, the DOTS, ambulatory, and hospital-based services were interrupted or compromised in all war-affected zones. These patients have a significantly higher risk of transmitting TB to others due to displacement and disruption of the DOTS system. Additionally, the likelihood of developing new drug resistance is high due to drug interruption. With the unprecedented struggle, the transmission of drug-resistant forms of TB was very low over the years in Ethiopia. According to the 2021 WHO Global TB Report, Ethiopia was removed from the list of high MDR-TB burden countries 2. However, the war caused treatment interruptions for thousands of people. This situation is expected to increase the incidence of drug-resistant TB in the country. Taken together, war creates perfect evolutionary pressure for TB transmission and resistance. Unless concerted efforts are made to trace cases and contacts, the situation will paralyze the national health system.
Tuberculosis is a major cause of preventable suffering and death among women 15. In this study, severe forms of TB disproportionately affect women and children. In the region, the proportions of EPTB, clinically confirmed TB cases, and pulmonary TB cases among females were 49.32%, 26.64%, and 24.04%, respectively. Evidence also documents that women are at an increased risk of disease progression during their reproductive years 16. Biological mechanisms may account for most of this difference. Tuberculosis control programs should be sensitive to the constraints faced by women in accessing healthcare. However, significant under-detection of TB is more common in females than in males 17. Moreover, a major challenge in estimating the burden is under-reporting and diagnostic uncertainties 17.
In this study, severe TB mainly affects the economically disadvantaged segments of the population, specifically children and women of reproductive age. The morbidity and mortality resulting from the indirect and lingering effects of wars are approximately equal to those incurred directly and immediately from all wars. This impact manifests through specific diseases and conditions, disproportionately affecting women and children 18. The Bacille Calmette–Guérin (BCG) vaccination is administered to children to prevent severe forms of TB. It is claimed that mass BCG vaccination, especially at school-leaving age, can yield benefits not only directly by protecting individuals from TB but also indirectly by breaking the chain of transmission and preventing the spread of tuberculosis 19. However, BCG vaccination coverage is low or even zero in conflict-affected zones. This situation might exacerbate the emergence of severe forms of TB (EPTB) in the region, surpassing its pre-war status.
The war in the Amhara region has significantly impacted tuberculosis case notification and treatment. Before the conflict, there was a steady increase in TB treatment outcomes and a stable case detection rate in the war-affected areas of the Amhara National Regional State. However, due to interruptions in TB care in these zones, the TB notification rate and treatment outcomes have dramatically decreased. This situation could lead to a manifold increase in TB transmission in war-affected areas and IDP centers, where more than five million people reside. For instance, there were 85,403 TB cases in the war-affected areas, and individuals were displaced without triaging their TB status, potentially spreading the disease among healthy individuals. Moreover, out of 116 drug-susceptible TB patients identified, 85 (73.3%) were from IDP sites. This creates a conducive environment for TB transmission in IDP sites and the war-affected community. Evidence suggests that an individual with TB could transmit the disease to approximately 15 healthy persons. Based on this calculation, more than one million new TB cases could potentially be added to the existing TB burden 20. The number could potentially exceed fifteen in IDP centers due to delays in diagnosis and treatment initiation, as well as unsuccessful outcomes in TB treatment 11. Amid the ongoing war and conflict, forced displacement is widespread, leading to overcrowded detention centers. The development of chronic malnutrition and hunger is inevitable, drug interruptions are likely, and infection prevention mechanisms are likely compromised 21. These collective conditions not only facilitate transmission and reactivation but also increase the likelihood of mortality and the development of multidrug-resistant (MDR) and extensively drug-resistant (XDR) TB. The majority of patients with drug-resistant TB also face various psychosocial and economic challenges 22,23.
In the present study, five patients with drug resistance were diagnosed. The quality of life of MDR-TB patients was compromised across physical, psychological, environmental, and social domains. Additionally, a study indicated that 23% of MDR-TB patients had defaulted on treatment due to financial constraints 24. Collectively, TB, especially drug-resistant TB, significantly impacts the productivity of the population. These challenges underscore the profound implications of the war on TB control programs in the Amhara region.
The incidence of TB was notably high in war-affected areas. Severe forms of TB and underdiagnosed cases were more prevalent, contributing to increased TB transmission, reactivation, and the development of drug resistance in both affected and unaffected zones. The regional TB prevention and control program faced severe limitations and was overwhelmed by forced displacements. Therefore, enhancing active and passive case finding, restoring diagnostic capabilities, ensuring BCG vaccination, implementing rigorous TB screening and surveillance, and managing TB, including severe forms like MDR-TB and XDR-TB, are crucial measures to strengthen the regional TB control program.
Authors would like to thank data collectors, zonal health department TB officers and the Amhara Public Health Institute
ANRS…Amhara National Regional State BCG… Bacillus Calmette-Guérin DOTS…Directly Observed Therapy Short course HMIS…Health Management Information System IDP…Internally Displaced Persons LQAS…Lot Quality Assurance Sampling MDR…Multidrug-resistant MDR-TB… Multidrug-resistant TB PTB+…Pulmonary TB positive RR…Rifampicin Resistance TB…Exacerbating Tuberculosis WHO…World Health Organization ZN…Ziehl-Neelsen
Prior to the study, ethical approval was obtained from the Ethical Review Board of Amhara Public Health Institute. Permission to access data was granted through written letters from APHI. Informed written consent was obtained from respondents who participated in the post-war assessment. Data were solely used for the purpose of the study, and all personal identifiers were removed to ensure confidentiality and anonymity.
Not applicable.
All the datasets analyzed during the current study are available from the corresponding author upon reasonable request.
Authors have no competing interests
No funding
All authors contributed equally
MB: MSc in Infectious and Tropical Diseases, MW: MPH in Field Epidemiology; BB: MPH in Field Epidemiology, GD: PhD in Public Health and Professor, MY: PhD in Public Health and Professor of Health Systems and Policy, AA: MSc in Pharmacy, BBA: MPH in Field Epidemiology, Daniel Mekonnen: PhD in Health Biotechnology; DA: MSc in Pediatric and Child Health; DS: MSc in Biomedical Sciences, GMA: MPH, KA: MSc in Epidemiology and Biostatistics, MM: MSc in Information Technology, MT: MPH, TZ: MPH, and GY: PhD in Medical Sciences