Prevalence and Determinants of Anemia among Pregnant Women in Ethiopia: a Multilevel Analysis
1 Research and Development Directorate, Amhara Public Health Institute, Bahir Dar, Ethiopia
2Department of Statistics, College of Natural and Computational Sciences, Debre Tabor University, Ethiopia
3Department of Statistics, College of Science, Bahir Dar University, Ethiopia
4Departement of Nutrition and Dietetics, School of Public Health College of Medicine and Health Sciences, Bahir Dar University
* Corresponding Author: Girum Meseret Ayenew: Email: girum.m21@gmail.com, Bahir Dar, Ethiopia,
Background: Anemia is a significant global public health problem that particularly affects pregnant women. According to the World Health Organization, 40% of pregnant women are anemic worldwide. This study is aimed at determining the prevalence and identifying determinants of anemia among pregnant women in Ethiopia.
Methods: Ethiopian demography and health survey of 2016 data were used for the analysis. A total of 1,122 pregnant women were included in the analysis. A multi-level proportional odds model was used to identify the determinant factors of anemia among pregnant women.
Result: The prevalence of anemia among pregnant women in Ethiopia was 41.35%. The random effect model revealed that 89.06% of the variability of anemia among pregnant women explained by individual and community level factors. The multilevel proportional odds model revealed that level of education, consumption of iron folate tablets, income and birth interval were significantly associated with lower prevalence of anemia. However, number of living children, latrine facilities and region of residency were associated with the higher prevalence of anemia. Pregnant women living in Afar, Benishangul-Gumuz, Gambella, SNNPR and Dire Dawa regions had higher prevalence of anemia.
Conclusions: The prevalence of anemia among pregnant women in Ethiopia was high. Anemia prevention strategies need to be targeted on women with low educational level, low economic status, areas with poor latrine facilities, larger number of living children’s women and short birth spacing women.
Keywords: Anemia, pregnant women, multilevel analysis, Ethiopia
የጥናቱ ዳራ፡ የደም ማነስ በተለይም ነፍሰ ጡር እናቶችን የሚያጠቃ ዓለም አቀፍ የህዝብ ጤና ችግር ነው። የዓለም ጤና ድርጅት እንደገለጸው በዓለም ዙሪያ 40 በመቶ የሚሆኑ ነፍሰ ጡር እናቶች የደም ማነስ ችግር አለባቸው። ይህ ጥናት በኢትዮጵያ ነፍሰ ጡር እናቶች ላይ ያለውን የደም ማነስ ስርጭት ለማወቅ እና ወሳኝ ሁኔታዎችን ለመለየት ያለመ ነው።
የጥናቱ ስልት/ዘዴ: የ2016 የኢትዮጵያ የስነ ህዝብ እና የጤና ዳሰሳ ጥናት ለትንታኔው ጥቅም ላይ ውሏል። በጠቅላላው 1,122 ነፍሰ ጡር እናቶች በጥናቱ ተካተዋል። የደም ማነስን የሚወስኑ ምክንያቶችን ለመለየት ባለብዙ ደረጃ ተመጣጣኝ ሞዴል ጥቅም ላይ ውሏል።
የጥናቱ ዉጤት፡ በኢትዮጵያ ነፍሰ ጡር እናቶች የደም ማነስ ስርጭት 41.35 በመቶ ነበር። ሞዴሉ እንደሚያሳየው ሞዴል በነፍሰ ጡር ሴቶች መካከል ያለው የደም ማነስ ልዩነት ምክንያቶች 89.06 በመቶ በግለሰብ እና በማህበረሰብ ደረጃ ተብራርቷል። የትምህርት ደረጃ ፣ የአይረን ፎሌት ኪኒኖች ፍጆታ ፣ የገቢ መጠን እና የወሊድ ጊዜ መራራቅ ከዝቅተኛ የደም ማነስ ስርጭት ጋር በእጅጉ የተቆራኙ መሆናቸውን ያሳያል። ነገር ግን ፣ በሕይወት ያሉ ሕጻናት ቁጥር ፣ የመጸዳጃ ቤት መገልገያዎች እና የመኖሪያ ክልል ከከፍተኛ የደም ማነስ ስርጭት ጋር ተያይዘዋል። በአፋር ፣ በቤኒሻንጉል ጉሙዝ ፣ በጋምቤላ ፣ በደቡብ ክልል እና በድሬዳዋ ክልሎች የሚኖሩ ነፍሰ ጡር እናቶች ከሌሎች ክልሎች በተለየ ሁኔታ ከፍተኛ የደም ማነስ ችግር ታይቶባቸዋል።
የጥናቱ ማጠቃለያና ምክረ ሀሳብ፡ በኢትዮጵያ ነፍሰ ጡር እናቶች የደም ማነስ ስርጭት ከፍተኛ ነው። ዝቅተኛ የትምህርት ደረጃ ያላቸው፣ ዝቅተኛ የኢኮኖሚ ደረጃ ያላቸው፣ ደካማ መጸዳጃ ቤት ባለባቸው አካባቢዎች፣ በሕይወት ያሉ ሕጻናት ያላቸው እናቶች እና የተቀራረበ የወሊድ ክፍተት ባላቸው እናቶች ላይ የደም ማነስ መከላከል ስትራቴጂዎችን ማነጣጠር ያስፈልጋል።
ቁልፍ ቃላት፡ የደም ማነስ፣ ነፍሰ ጡር እናቶች ፣ ባለ ብዙ ደረጃ ትንተና ፣ ኢትዮጵያ
Anemia refers to a low haemoglobin level (<110g/L for pregnant women). If an individual’s haemoglobin level is low, the red blood cells are unable to carry adequate oxygen for the body’s physiological needs.1 Anemia impairs physical health, cognitive development, and productivity and reflects the poor economic development of a country. Anemia is a major public health problem in women. Worldwide, 38% of pregnant women were anemic in 2011.2 Pregnant women in low and middle-income countries experience high rates of anemia, in which the highest prevalence rates are reported in Central and West Africa (56%), South Asia (52%) and East Africa (36%).2 Anemia can have negative effects on a woman’s health including maternal mortality and severe morbidity.3 as well as negative influences on the infant including birth weight and preterm birth.4 Reducing anemia is considered as an essential part of improving the health of women, and WHO has set a global target of achieving 50% reduction of anemia among pregnant women by 2025.5 Anemia is also a common problem in Ethiopia; the recent Ethiopian Demographic Health Survey (EDHS2016) reported 29% prevalence of anemia among pregnant women and the prevalence rate ranging from 16% to 59% across different parts of the country.6 There are a number of different factors contributing to the prevalence of anemia, with iron deficiency the maincause.7 Other micronutrients (vitamin A, vitamin B12 and folate), chronic bleeding, acute or chronic infections and parasitic infections (hookworm and malaria) are also known to cause anemia.8, 9
Earlier studies conducted in Ethiopia to analyze the odds factors for anemia among pregnant women was institutional-based.10-13 and only looked at individual-level factors.10,11, 14 ,15 However, pregnant women's anemia may be affected by group-level factors, such as latrine facilities.16, 17 water source,16 level of education18,residence,19 region19 and cluster (enumeration area).18 Besides, the above studies used binary logistic regression model to explore the determinants of anemia. The response variable for the above studies was considered as binary (anemic and not anemic); as a result, the binary logistic regression model did not take into account the anemia severity. To address this, we used the ordinal logistic regression model to identify the odds factors of anemia among pregnant women.
Furthermore, using a standard ordinal regression analysis method to analyze data in a hierarchical design (i.e., women nested within households and households nested within communities) violates the regression’s independence assumptions. This study used a multilevel proportional odds regression model to overcome these drawbacks and to predict the true impact of the above-mentioned factors on multilevel determinants of anemia in order to incorporate more successful future healthcare measures that target specific unit at different levels of the hierarchy and there could be a correlation between the higher levels. Therefore, this study aimed to determine the prevalence and identify the determinants of anemia among pregnant women in Ethiopia using multilevel proportional odds model.
A study was conducted in Ethiopia, which is situated in the North-Eastern part of Africa, also known as the horn of Africa. This study used a publicly available EDHS 2016 dataset which was conducted by the Central Statistical Agency (CSA). EDHS 2016 was a population-based cross-sectional study conducted across the country. It is the fourth national survey conducted in all parts of Ethiopia (in nine regional states and two city administrations.6 In Ethiopia, the states are administratively further subdivided into zones, zones into Woredas and Woredas further into the lowest unit called Kebeles.
In the 2016 EDHS, stratified and cluster multistage sampling was used, and it was intended to be representative at the regional and national level in terms of appropriate demographic and health indicators. In the first stage, 645 clusters of enumeration areas (EAs) (202 urban and 443 rural) were identified using probability proportional to the size of EAs. In the second stage, random samples of 18,008 households were selected from all the identified EAs. Lastly, 15683 women (15–49 years) were successfully interviewed, yielding a response rate of 98%. A total of 1122 currently pregnant women were included in this study.6 Data collection took place from 18 January 2016 to 27 June 2016. The sample size for EDHS was calculated using a multistage sampling technique that took into account sampling variation.
The outcome variable of this study was the anemic status of pregnant women. Hemoglobin levels of the women were measured using hematocrit value, which is the standard test used in the EDHS 2016. Pregnant women with a hematocrit value greater than 33% was considered as non-anemic, 30%-33% as mild anemia, 21%-30% as moderate anemia and less than 21% as severe anemia
Determinants of anemia were categorized as individual, household and community level factors. Those factors were selected based on various works of literature,10,14,20,21 and theoretical justification. Individual factors included age, religion, marital status, educational status, body mass index, birth interval, use of contraceptives, wealth index, household size, iron-folate intake and gravidity of women, while the household level factors were residence (urban and rural), region, water source and latrine facility type. Community-level factors like community wealth index, community level women education, community level ANC utilization, community level water sources and community level latrine facility type. At the cluster level, the community-level factors are formed by aggregating the selected individual and household-level factors (not directly found in the EDHS). The aggregates were computed using the percentage of a particular variable's subcategory in a given cluster because the aggregate value for all generated variables was not normally distributed. Based on their median values, it was divided into two categories (low and high proportion).18, 22
Data were extracted and the analysis was performed by using R software version 3.5.3. Descriptive statistics including frequencies, percentages, and bar chart were performed to describe the study participants. The 2016 EDHS data are hierarchical nature and were collected using stratified multi-stage cluster sampling. Thus, data have a three-level hierarchical structure with pregnant women (level 1) nested within households (level 2) nested within clusters (level 3). Pregnant women in one cluster may have similar characteristics to those in another. The ordinal logistic regression model's observations of independence and equal variance between clusters are violated. As a result, an advanced model must be used to account for cluster heterogeneity. As a result, to obtain a valid estimate and standard error, a multilevel proportional odds model was used. This study used a three-level proportional odds model to identify determinants of anemia among pregnant women. Chi-square parallel line tests carried out to assess the validity of the proportional odds assumption. For this multilevel proportional odds model analysis, five models were constructed. The first model was constructed without independent variables to assess the effect of community variation on anemia among pregnant women. Individual-level factors were incorporated in the second model. In the third model, household-level factors were included. Community-level factors were included in the fourth model. Finally, individual-level, household-level and community-level factors were included in the fifth model. The Deviance Information Criteria (DIC) and Akaike's Information Criterion (AIC) were used to compare the candidate models and the model with the minimum information criteria was considered as the best-fitting model.23
The results of the fixed effect were reported as Adjusted Odd Ratios (AOR). The AOR with 95% CI and p<0.05 in the multivariable model were used to reveal significantly associated factors of anemia among pregnant women. The Intra-Cluster Correlation Coefficient (ICC), Median Odds Ratio (MOR), and proportional change in variance (PCV) were used to determine the random effects. MOR can quantify unexplained cluster variability, whereas ICC can explain cluster variability (heterogeneity). PCV can assess the overall variation attributable to community and individual-level factors in the multilevel model. The following formula was used to determine the ICC, PCV, and MOR:
where VA is the estimated variance in each model, which has been described elsewhere. 24
![]() where VA = variance of the initial model, and VB = variance of the model with more terms .24
where VA = variance of the initial model, and VB = variance of the model with more terms .24
![]() , where VA is the cluster level variance.24,25
, where VA is the cluster level variance.24,25
A total of 1,122 pregnant women were included in the analysis. More than half, 616 (54.9%) of the respondents were in the age group between 20 and 29 years and 633 (56.4%) had no formal education. Nearly three-fourth, 831 (74.1%) of the respondents were unemployed in the last twelve months prior to the survey and about half, 590 (52.6%) had households of 6 or more people. About 18% (n=196) of the respondents had attended ANC at least four times during pregnancy and most (924; 82.4%) delivered at home. The majority, 885(78.9%) women were rural dwellers and 586(52.2%) of the women were from households with poorest wealth index. About forty percent (n=448) of women used unimproved sources of drinking water and 55.9 % of women used latrine facility. Furthermore, 62.5% of the pregnant women were living in communities with a lower proportion of maternal education and 56.2% of the pregnant women from communities with a lower proportion antenatal care visit (Table 1).
Table 1. Socio-demographic and health characteristics of participants
| Variables | Frequency | Percentage |
|---|---|---|
| Age of women | ||
| 15-19 | 117 | 10.4 |
| 20-29 | 616 | 54.9 |
| 30-39 | 348 | 31 |
| 40-49 | 41 | 3.7 |
| Educational status | ||
| No education | 633 | 56.4 |
| Primary | 333 | 29.7 |
| Secondary and above | 156 | 13.9 |
| Occupational status | ||
| Not working | 831 | 74.1 |
| Working | 291 | 25.9 |
| Smoking | ||
| No | 1,109 | 98.8 |
| Yes | 13 | 1.2 |
| Number of antenatal visits | ||
| No antenatal visits | 707 | 63 |
| 3-Jan | 219 | 19.5 |
| 4 and above | 196 | 17.5 |
| Place of delivery | ||
| Home | 924 | 82.4 |
| Health facility | 198 | 17.6 |
| Iron supplementation | ||
| No | 834 | 74.3 |
| Yes | 288 | 25.7 |
| Drugs for intestinal parasites | ||
| No | 1,075 | 95.8 |
| Yes | 47 | 4.2 |
| Birth interval (months) | ||
| <24 | 655 | 58.4 |
| >=24 | 467 | 41.6 |
| Family size | ||
| less than 3 | 176 | 15.7 |
| 4-Mar | 356 | 31.7 |
| greater than 4 | 590 | 52.6 |
| Wealth index | ||
| Poor | 586 | 52.2 |
| Middle | 148 | 13.2 |
| Rich | 388 | 34.6 |
| Current pregnancy wanted | ||
| Then | 897 | 79.9 |
| Later | 155 | 13.8 |
| Not at all | 70 | 6.2 |
| Ever had terminated pregnancy | ||
| No | 1,004 | 89.5 |
| Yes | 118 | 10.5 |
| Currently breastfeeding | ||
| No | 1,042 | 92.9 |
| Yes | 80 | 7.1 |
| marital status | ||
| Married | 1,081 | 96.3 |
| Others | 41 | 3.7 |
| Age at first sex | ||
| <15 | 410 | 36.5 |
| >15 | 712 | 63.5 |
| Number of living children | ||
| 0-2 | 657 | 58.6 |
| 4-Mar | 280 | 25 |
| >5 | 185 | 16.5 |
| Water source | ||
| Piped water | 188 | 16.8 |
| Other protected | 486 | 43.3 |
| Unprotected | 448 | 39.9 |
| Type of latrine facility | ||
| Improved latrine | 627 | 55.9 |
| Unimproved latrine | 495 | 44.1 |
| Region | ||
| Tigray | 80 | 7.1 |
| Afar | 120 | 10.7 |
| Amhara | 103 | 9.2 |
| Oromia | 155 | 13.8 |
| Somali | 185 | 16.5 |
| Benishangul | 81 | 7.2 |
| SNNPR | 144 | 12.8 |
| Gambella | 64 | 5.7 |
| Harari | 85 | 7.6 |
| Addis Ababa | 47 | 4.2 |
| Dire Dawa | 58 | 5.2 |
| Place of residence | ||
| Urban | 237 | 21.1 |
| Rural | 885 | 78.9 |
| Community level latrine facility type | ||
| Improved latrine | 601 | 53.6 |
| Unimproved latrine | 521 | 46.4 |
| Community level wealth index | ||
| Low | 605 | 53.9 |
| High | 517 | 46.1 |
| Community level women education | ||
| Low | 701 | 62.5 |
| High | 421 | 37.5 |
| Community level ANC utilization | ||
| Low | 631 | 56.2 |
| High | 491 | 43.8 |
| Community level water sources | ||
| Protected water sources | 647 | 57.7 |
| Unprotected water sources | 475 | 42.3 |
The prevalence of anemia among pregnant women in Ethiopia was 41.35% (95% CI: 38.45% to 44.30%) and among these 9% (95% CI: 7.39% to 10.83%) was severely anemia, 16.20% (95% CI: 14.11% to 18.51%) were moderately anemia and 16.10% (95% CI: 14.03% to 18.42%) were mild anemia (Figure. 1).
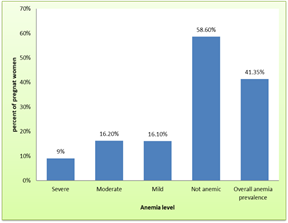
Figure 1. Prevalence of anemia among pregnant women in Ethiopia.
The result of fixed effect model was presented in Table 2. The score test of proportional odds assumption is found not significant at 5 % level of significance (Table 3); this means that the proportional odds assumption is satisfied. The final selected model (model V) showed that maternal education, Iron supplementation during pregnancy, wanted pregnancy, wealth index, birth interval, number of living children, type of latrine facility, region, community level wealth index, community level maternal education and community level type of latrine facility use were factors significantly associated with anemia among pregnant women (Table 2 and Table 3)
The odds of having severe anemia was 0.595 (AOR =0.595, 95%CI: 0.435, 0.813) and 0.556 (AOR =0.556, 95%CI: 0.365, 0.848) times lower for women attended primary education and secondary or higher education respectively as compared to women with no formal education. The odds of being mild anemic in pregnant women who took iron pills was 0.482 (AOR =0.482, 95%CI: 0.279, 0.832) times than pregnant women who didn’t take iron pills. Women who had more than two years’ pregnancy interval were 0.713 (AOR =0.713, 95%CI: 0.542, 0.938) times less likely to develop anemia than women who had short pregnancy interval. The odds of having severe anemia status 0.484 (AOR =0.484, 95%CI: 0.260, 0.903) times higher among the unwanted current pregnancy, when compared to wanted pregnancy (Table 2).
The odds of developing lower odds of anemia in pregnant women from household with middle income was 0.550 (AOR =0.550, 95%CI: 0.359, 0.840) times than poorest pregnant women. Besides, the odds of developing lower odds of anemia in pregnant women from richest household was 0.655(AOR =0.655, 95%CI: 0.465, 0.924) times than poorest pregnant women. Pregnant women having birth interval 24 months and above had 0.713 (AOR =0.713, 95%CI:0.542, 0.938) times lower odds of having worse anemia status compared with the women having birth interval of fewer than 24 months. Pregnant women from households without access to a latrine was 1.508 (AOR =1.508, 95%CI: 1.128, 2.016) times more likely to be in severe anemia status as compared with women from households that had an improved latrine facility. The odds of having severe anemia status were 1.516 (AOR =1.516, 95%CI:1.134, 2.027) higher among mothers who had given birth to three up to four children, when compared to mothers who had given birth fewer than three children (Table 2).
Pregnant women live in Afar (AOR=3.950; 95% CI: 2.051, 7.609), Oromia (AOR=2.533; 95% CI: 1.320, 4.861), Somali (AOR=8.707; 95% CI:4.642,16.331), Benishagul-Gumz (AOR=2.680; 95% CI:1.288,5.576), SNNPR (AOR=2.049; 95% CI:1.051,3.996), Harari (AOR=5.720; 95% CI:2.830, 11.562) and Dire Dawa (AOR=5.339; 95% CI: 2.467, 11.556) were times more likely to be in severe anemia status as compared to women live in Tigray. Pregnant women living in communities with high level of maternal education had a 33% (AOR=0.670; 95% CI: 0.474, 0.947) of lower likelihood of developing anemia as compared to those women living in communities with high maternal education level. Pregnant women residing in communities with a high proportion of wealth index had 40.4% (AOR =0.596; 95% CI: 0.427, 0.832) higher odds of experiencing anemia as compared to women residing in communities with a low proportion of wealth index. Pregnant women living in communities without access to a latrine were 1.527 (AOR=1.527; 95% CI:1.137, 2.047) times more likely to be in severe anemia status as compared to those women living in communities having an improved latrine facility (Table 2).
Table 2. Individual, household and community level factors associated with anemia status among pregnant women using multilevel ordinal logistic regression analysis.
| Variables | Model II | Model III | Model IV | Model V |
|---|---|---|---|---|
| AOR (95% CI) | AOR (95% CI) | AOR (95% CI) | AOR (95% CI) | |
| Educational status | ||||
| No education | ||||
| Primary | 0.578(0.418, 0.798)* | 0.595(0.435, 0.813)* | ||
| Secondary and above | 0.501(0.323, 0.775)* | 0.556 (0.365, 0.848)* | ||
| Iron supplementation | ||||
| No | ||||
| Yes | 0.527 (0.301, 0.923)* | 0.482(0.279, 0.832)* | ||
| Current pregnancy wanted | ||||
| Then | ||||
| Later | 0.772 (0.524, 1.138) | 0.962(0.662,1.397) | ||
| Not at all | 0.308 (0.161, 0.587)* | 0.484(0.260, 0.903)* | ||
| Wealth index | ||||
| Poor | ||||
| Middle | 0.516(0.339, 0.786)* | 0.550 (0.359, 0.840)* | ||
| Rich | 0.600(0.438 , 0.820)* | 0.655 (0.465, 0.924)* | ||
| Birth interval (months) | ||||
| <24 | ||||
| >24 | 0.678(0.508,0.905)* | 0.713 (0.542,0.938)* | ||
| Number of living children | ||||
| 0-2 | ||||
| 4-Mar | 1.638(1.183 ,2.270)* | 1.508(1.128, 2.016)* | ||
| >5 | 1.117(0.766,1.630) | 0.974(0.684, 1.385) | ||
| Type of toilet facility | ||||
| Improved toilet | ||||
| Unimproved toilet | 1.656(1.231,2.227*) | 1.516(1.134, 2.027)* | ||
| Region | ||||
| Tigray | ||||
| Afar | 4.043(2.089,7.825)* | 3.950(2.051,7.609)* | ||
| Amhara | 0.713(0.332,1.533) | 0.774(0.361, 1.656) | ||
| Oromia | 2.346(1.220,4.512)* | 2.533(1.320, 4.861)* | ||
| Somali | 8.621(4.593,16.184)* | 8.707(4.642, 16.331)* | ||
| Benishangul | 2.657(1.273,5.544)* | 2.680(1.288, 5.576)* | ||
| SNNPR | 1.943(0.993,3.802) | 2.049(1.051, 3.996)* | ||
| Gambella | 1.999(0.928, 4.305) | 2.039(0.950, 4.374) | ||
| Harari | 5.702(2.802, 11.604)* | 5.720(2.830, 11.562)* | ||
| Addis Ababa | 1.348(0.547, 3.320) | 1.561(0.634, 3.843) | ||
| Dire Dawa | 5.144(2.364, 11.189)* | 5.339(2.467, 11.556)* | ||
| Community level toilet facility type | ||||
| Improved toilet | ||||
| Unimproved toilet | 1.794 (1.328, 2.424)* | 1.524(1.137, 2.043)* | ||
| Community level wealth index | ||||
| Low | ||||
| High | 0.472(0.320, 0.696)* | 0.596 (0.427, 0.832)* | ||
| Community level education | ||||
| Low | ||||
| High | 0.624(0.437, 0.890)* | 0.670 (0.474, 0.947)* |
The result of the random effect model and the model fitness is summarized in Table 3. The empty model revealed that 21.9% of the total variability for anemia was due to differences between household and community-level factors, with the remaining unexplained 78.1% which was attributed by individual differences. Besides, the empty model also had the highest MOR value (2.49) showed there was a variation of anemia between clusters since MOR was 2.49 times higher than the reference (MOR=1). Moreover, the highest (89.06%) PCV in the final full model (Model V) indicates that 89.1% of the variation in anemia across communities was explained by individual, household and community level factors. AIC and Deviance statistics were used to identify the appropriate multilevel model among the five commonly considered consecutive models. The final full model (Model V) has the smallest AIC and Deviance statistic. This indicates that final full model (Model V) was a better fit to data as compared to the other reduced models (Table 3).
Table 3. Measures of variation and model fit statistics in anemia status among pregnant women.
| Measure of variation | Model I | Model II | Model III | Model IV | Model V |
|---|---|---|---|---|---|
| Variance (SE) | 0.923 (0.249)* | 0.676 (0.221)* | 0.732(0.223)* | 0.147 (0.137)* | 0.101 (0.131)* |
| PCV (%) | Reference | 26.76 | 20.69 | 47.35 | 89.06 |
| ICC (%) | 21.91 | 17.04 | 18.2 | 12.87 | 2.98 |
| MOR | 2.49 | 2.18 | 2.25 | 1.94 | 1.35 |
| Score test for proportional odds assumption | X2(5) =6.071, | X2(6) = 8.591, | X2(13) =19.607, | X2(24) =23.103, | |
| P-value=0.551 | P-value=0.072 | P-value=0.791 | P-value=0.084 | ||
| Model fit statistics | |||||
| DIC (-2log likelihood) | 2479.2 | 2446.97 | 2447.23 | 2345.95 | 2324.94 |
| AIC | 2487.2 | 2464.97 | 2467.23 | 2375.95 | 2364.95 |
The global burden of anemia among pregnant women is widely acknowledged as a major public health issue, especially in developing countries. Hemoglobin levels changed drastically during pregnancy due to blood volume expansion and elevated iron demand of the fetus and mother. In Ethiopia, the prevalence of anemia among pregnant women was 41.35%. This result is higher than 25.75% in Damaturu Nigeria, 26 29.4% in Kabgayi Hospital, Rwanda,27 25% in Sho’ub District of Sana’a City, Yemen,28 though it is lower than 66.9% in Nepal.29 This may be attributable to differences in the sample size of the study, socio-demographic characteristics of the respondents, access of health care, study time, latrine coverage, and utilization.
According to the random-effects logistic regression model, the variation in the anemia among pregnant women was attributed to both individual- and community-level factors. The proportional change in variance for the final full model (model IV) revealed that both individual- and community-level factors accounted for about 89.06% of the variation observe for anemia among pregnant women. This finding is in line with studies conducted in Eastern Africa 16 and sub-Saharan Africa. 30
When compared to rich women, poor women had a higher odd of developing severe anemia (as opposed to moderate, mild, or non-anemic). This result is consistent with studies conducted in Eastern Africa,16 Ethiopia14, 17, 31 Nigeria,32 and sub-Saharan Africa. 30 The poor women may have less money to afford healthy foods or have a regular diet, which contributes to insufficient nutrient consumption and nutritional status. Women who received iron during pregnancy were less likely to experience severe anemia (against to moderate, mild, or non-anemic) than women who did not receive iron. This finding was in agreement with a study done in Cameron.20
Relative to educated women, uneducated women were more likely to suffer from severe anemia (as opposed to moderate, mild, or non-anemic).This is in line with the studies carried out in eastern Africa,16 Nepal,19, 29 and Nigeria.32 This may be attributed to the fact that uneducated women's lower socioeconomic status, unhealthy lifestyle, and lack of disease preventive knowledge and skills relative to educated women. Besides, Education can help women gain information, which in turn allows them to adopt healthy lifestyle behaviors such as good nutrition and to form healthier health-seeking habits and hygiene practices, both of which can help avoid anemia in women.
Women with a longer pregnancy interval were less likely to experience anemia than women with a shorter pregnancy interval. This result is consistent with studies done in Ethiopia,31 and West Shewa zone, Oromia regional state, Central Ethiopia.10 This could be explained by the impact of the mother's overall physiologic status on the repeated and short inter-pregnancy intervals and breastfeeding31.The woman would not have enough time to recover from nutritional deficiency. 33
Women with a larger (3-4) number of living children were more likely to develop severe anemia (as opposed to moderate, mild, or non-anemic) than those with fewer (<2) number of living children. The finding was consistent with the previous studies done in Ethiopia,14 West Shewa zone, Oromia regional state, Central Ethiopia,10 and seven South and Southeast Asian countries. 34 Having a large number of living children is correlated with a poor socioeconomic status of the household, so there might be little food available to feed the whole family. Furthermore, a high number of live children are a good predictor of short birth spacing, which influences the maternal hemoglobin status.
Pregnant women who did not have access to a toilet were more likely to develop severe anemia (against to moderate, mild, or non-anemic) than women who had access to a toilet. This finding is supported by a study done in Ethiopia,17 Eastern Africa,16 and seven South and Southeast Asian countries.34
Higher maternal education at the community level was associated with a lower odd of serious anemia (against moderate, mild or non-anemic). Besides, having access to a toilet facility in the community can help to reduce the odds of serious anemia (as opposed to moderate, mild, or non-anemic) in that community. Moreover, women who lived in communities with a high proportion of wealth index had a lower odd of having severe anemia (as opposed to moderate, mild, or non-anemic) than women who lived in communities with a low proportion of wealth index. This finding is consistent with a study done Ethiopia 18 and seven South and Southeast Asian countries. 34
The geographical region was a significant predictor of anemia. Women living in Afar, Benishangul, Gambella, SNNPR, and Dire Dawa regions were more likely to be affected by anemia as compared to women living in Tigray. This finding is consistent with a study done in Ethiopia.18,31
The study used nationally representative DHS data collected from 2016. This helps to provide better representative data as all regions and administrative cities in the country were included. In addition, multilevel modeling was used to account for the hierarchical nature of the EDHS data. The causal effect is difficult to measure due to the cross-sectional structure of the data, and it is impossible to determine whether the data is time dependent or not.
Conclusion in Ethiopia, the prevalence of anemia in pregnant women differed by cluster (enumeration area). Therefore, anemia prevention strategies need to be targeted on women with low education level, low economic status, areas with poor latrine facilities, larger number of living children’s women and short birth spacing women in order to reduce the high incidence of anemia among pregnant women in Ethiopia. Meanwhile, Policies and programs aimed at addressing enumeration area variations in anemia need to be formulated and their implementation must be strongly pursued.
The authors would like to thank the Central Statistical Agency of Ethiopia, for making the data freely available for research purposes.
AIC: Akaike’s information criterion;
AOR: Adjusted proportional odds ratio;
CI: Confidence intervals;
DIC: Deviance information criterion;
EAs: Enumeration areas;
EDHS: Ethiopian demographic and health survey;
ICC: Intra-cluster correlation;
MOR: Median odds ratio;
PCV: Proportional change in variance;
SNNPR: Southern Nations, Nationalities, and People Region
WHO; World Health Organization
The study used available secondary data accessed under the National Data Sharing and Accessibility Policy (NDSAP) of the Government of Ethiopia. The data set had no identifiable information on the survey participants; therefore, no ethical approval is required for this work.
This study used EDHS 2016 child data set and extracted the outcome and explanatory variables. Data is publicly available online from (https://dhsprogram.com/Data/). Correspondence and requests for data and materials should be addressed to S.M.
None declared.
The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
GMA and SMF drafted the proposal, did the analysis, wrote the results and prepared the manuscript. GMA, BBA, HMF, NF and SLH revised and critically reviewed the manuscript. All authors read and approved the final manuscript.
GMA has Masters in General Public Health.